Zinc - Another micronutrient with macro-functions in COVID-19
Dicken Weatherby, N.D. and Beth Ellen DiLuglio, MS, RDN, LDN
The ODX COVID-19 Series
- COVID-19: The pandemic that has become endemic
- COVID-19: Overlapping risk factors and chronic disease
- Nutritional status COVID-19: A covert factor in disease susceptibility
- COVID-19: Blood chemistry biomarker patterns - Clues and patterns lurking just under the surface
- COVID-19: Blood chemistry biomarker patterns - Down the research rabbit hole
- COVID-19: Blood Biomarkers - Neutrophils
- COVID-19: Blood Biomarkers - Albumin
- COVID-19: BloodBiomarkers - Cytokines
- COVID-19: Blood Biomarkers - Interleukin-6
- COVID-19: Blood Biomarkers - Interleukin-10
- COVID-19: Blood Biomarkers - Vitamin C
- COVID-19: Blood Biomarkers - Vitamin D
- COVID-19: Blood Biomarkers - Zinc
- Biomarker characteristics and blood type - help sharpen the COVID-19 clinical picture
- COVID-19: Initial indications and conventional interventions
- COVID-19: Long-term risk reduction - Naturopathic, functional medicine, and nutrition-based approaches to prevention
- A healthy diet is primary prevention for COVID-19
- You should have a gut feeling about COVID-19
- Beyond dietary food patterns…plant-based compounds may mitigate COVID-19 risk
- Targeted nutrition support in the battle against COVID-19
- Targeted nutrition support in COVID-19: Armed with vitamin C
- Targeted nutrition support in COVID-19: In sync with zinc
- Targeted nutrition support in COVID-19: Micronutrients and phytonutrients are important players
- Optimal Takeaways for improving immunity and reducing susceptibility to COVID-19
- Optimal - The Podcast: Episode 8 -Blood Biomarkers and Risk Factors for COVID-19 and its Comorbidities
Zinc is only needed in trace amounts in the body, but it participates in a wide range of metabolic processes. These include antioxidant reactions, neurobehavioral development, cellular growth, immunity, development, and activation of T-lymphocytes, and inhibition of viral replication.[1]
Zinc supports the integrity and barrier function of epithelial cells (e.g., skin and mucous membranes) which are compromised in zinc deficiency. Fortunately, supplementation can improve epithelial barrier integrity.[2]
Zinc can also help to reduce the cytokine storm characteristic of severe COVID-19 due to its modulation of T cell activity.[3]
Zinc deficiency will have notably negative effects on immunity:[4]
- Reduced activity of immune cells, e.g., impaired phagocytosis.
- Decreased critical neutrophil functions.
- Weakened natural killer cell function.
- Reduced lymphocyte number and activation.
- Diminished antibody production.
- Imbalanced T helper cell cytokine secretion with decreased IFN-gamma production.
- IFNs are immunostimulatory cytokines with antiviral activity.
- Increased thymic atrophy and consequent risk of infection.
- Zinc is crucial to counteract excessive inflammatory reactions…resulting in a reduced production of pro–inflammatory cytokines.
- Drugs can deplete zinc. For example, long–term use of some ACE–inhibitors like captopril, verapamil, and ramipril can significantly lower serum zinc levels.
- On the other hand, excess of zinc can also impair immune response by inhibiting T–lymphocyte and B–lymphocyte function, reducing intracellular pathogen destruction in macrophages or inducing an overload of regulatory T cells,
- This demonstrates that a balanced zinc homeostasis is critical for adequate immune functions.
Zinc and COVID-19
An estimated 16% of all deep respiratory infections are caused by zinc deficiency worldwide. Zinc deficiency is commonly observed in immunosuppression, asthma, COPD, pneumonia, cystic fibrosis, autoimmune disorders, diabetes, CVD, obesity, cancer, kidney disease, liver damage and cirrhosis, and in the elderly. Symptoms of zinc deficiency include[5] [6]
- Aching and pain in limbs
- Cough
- Diarrhea
- Fever
- Gastrointestinal disorders
- General weakness
- Growth retardation
- Immune system imbalance
- Impaired smell and taste
- Runny nose
- Skin disorders
- Sore throat
- Susceptibility to infections
- Weight loss
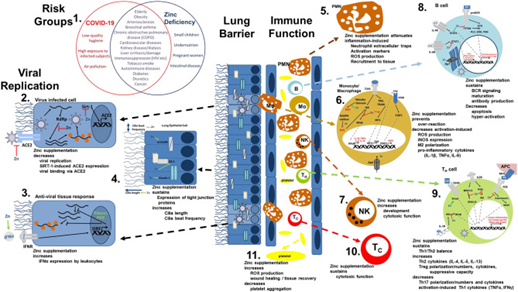
Source: Wessels, Inga et al. “The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis.” Frontiers in immunology vol. 11 1712. 10 Jul. 2020, doi:10.3389/fimmu.2020.01712 This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
Zinc and COVID-19 key points[vii]
- Zinc deficiency may be common and associated with severe infection.
- Zinc helps to enhance the interferon type 1 response to the virus and participates in many regulatory pathways.
- Low levels of zinc have been associated with higher IL-6 responses.
- IL-6 plays an important role in severe lung injury due to COVID-19 infection.
- Zinc inhibits SARS-CoV RNA polymerase, and thus its replication capacity.
- Zinc may increase the efficacy of antimalarial agents, since they are zinc ionophores.
- Differences in mortality due to COVID-19 infection may be explained to some degree by−174 IL-6 gene polymorphism
- Homeostasis maintains a constant intracellular zinc concentration and a plasma concentration within the reference range of 70-160 ug/dL (11–25 μmol/L). Low plasma zinc was defined as less than 60 ug/dL (less than 9.2 umol/L)
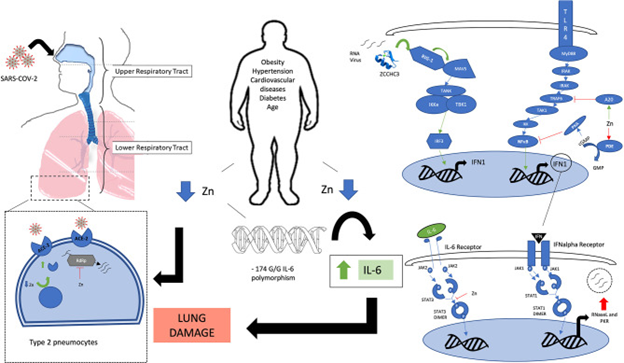
Source: Mayor-Ibarguren, Ander et al. “A Hypothesis for the Possible Role of Zinc in the Immunological Pathways Related to COVID-19 Infection.” Frontiers in immunology vol. 11 1736. 10 Jul. 2020, doi:10.3389/fimmu.2020.01736 This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms
A prospective study found significantly lower fasting serum zinc levels in 47 hospitalized COVID-19 patients with median serum levels of 74.5 ug/dL versus a median of 105. ug/dL in healthy controls. More than 57% of patients were blatantly zinc deficient with an odds ratio of 5.54 for developing complications including ARDS and prolonged hospital stay. Zinc deficiency was only observed in 11% of healthy controls with levels 71.8-79.6 ug/dL. Hospital reference ranges for zinc were 80-120 ug/dL (12.24-18.4 umol/L).[viii]
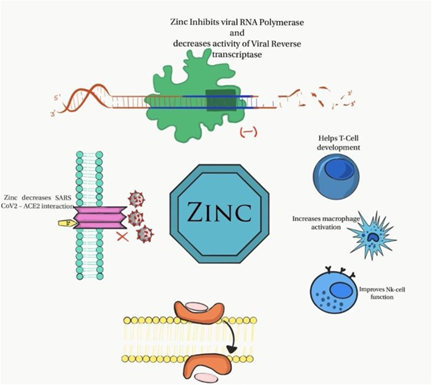
Illustration of antiviral and immunomodulatory properties of zinc in COVID-19.
Source: Jothimani, Dinesh et al. “COVID-19: Poor outcomes in patients with zinc deficiency.” International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases vol. 100 (2020): 343-349. doi:10.1016/j.ijid.2020.09.014 Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company's public news and information website. Elsevier hereby grants permission to make all its COVID-19-related research that is available on the COVID-19 resource centre - including this research content - immediately available in PubMed Central and other publicly funded repositories, such as the WHO COVID database with rights for unrestricted research re-use and analyses in any form or by any means with acknowledgement of the original source. These permissions are granted for free by Elsevier for as long as the COVID-19 resource centre remains active.
Zinc, along with vitamins C and D can have a synergistic effect in helping maintain the crucial first-line barriers of skin and mucous membranes. Insufficiency or marginal deficiency will disrupt metabolism and compromise immunity.[ix]
Zinc insufficiency, especially within immune cells, may be directly related to dysregulation of immune responses in the elderly who are at greater risk of zinc deficiency and COVID-19 morbidity. [x]
Researchers note that serum zinc below 70 ug/dL (10.7 umol/L) is considered a risk factor for pneumonia in the elderly. Reduced zinc also correlates with increased levels of IL-6, IL-8, and TNF-alpha. A daily preventative dose of 25 mg or less should be adequate. Intake of more than 25 mg/day may disrupt copper balance and warrant increased copper intake. Researchers also recommend selenium supplementation of 100-200 ug/day if serum levels are below 100 ug/L (1.27 umol/L).[xi]
Up to 79% of COVID-19 patients present with acute gastrointestinal complications including abdominal pain, vomiting, diarrhea, or gastrointestinal bleeding. Research suggests that supplementation with zinc amino acid chelate may help restore gastrointestinal integrity, resolve diarrhea, and replete zinc lost via the GI tract.[xii]
Researchers suggest that zinc supplementation may be beneficial to healing tissue damage caused by inflammation and the related cytokine storm seen during COVID-19.[xiii]
Hypogeusia (loss of taste) and hyposmia/anosmia (loss of smell) are significant findings in COVID-19 patients with 71-89% experiencing loss of taste and 68-85% experiencing olfactory dysfunction. These are recognized signs of zinc insufficiency as well. A study of 134 COVID-19 patients revealed that 78.4% of them had a loss of smell. Serum zinc levels in those with olfactory dysfunction were 57-59 ug/dL compared to 61-63 ug/dL in those without olfactory dysfunction, a non-statistically significant difference. However, zinc therapy with 50 mg elemental zinc twice daily did reduce the duration of olfactory dysfunction.[xiv]
It is notable that the range of serum zinc for all patients in this study (57-63 ug/dL) was below the optimal range of 80-100 ug/dL needed for the maintenance of homeostasis.[xv]
Researchers note that hypogeusia may occur without accompanying olfactory disturbances and may occur prior to organ or lung involvement in COVID-19, prompting calls for early supplementation with oral zinc lozenges in these patients.[xvi]
A suboptimal level of alkaline phosphatase may also be a clue to an underlying zinc (or magnesium) deficiency and should be part of a comprehensive nutrition assessment.[xvii]
Standard reference range serum zinc
Quest[xviii] 50-130 ug/dL
Labcorp[xix] 56-135 ug/dL
Optimal DX range 80 - 100 ug/dl
We cannot overlook the importance of zinc to immunity and our frontline defenses against COVID-19. Providing at least the minimum daily requirement of zinc can help ensure that the frontlines are fortified.
Next Up - COVID-19 & Blood Type
Research
[1] Jothimani, Dinesh et al. “COVID-19: Poor outcomes in patients with zinc deficiency.” International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases vol. 100 (2020): 343-349. doi:10.1016/j.ijid.2020.09.014
[2] Souza, Ana Carolina Remondi, et al. "Zinc, Vitamin D and Vitamin C: Perspectives for COVID-19 With a Focus on Physical Tissue Barrier Integrity." Frontiers in Nutrition 7 (2020): 295.
[3] Souza, Ana Carolina Remondi, et al. "Zinc, Vitamin D and Vitamin C: Perspectives for COVID-19 With a Focus on Physical Tissue Barrier Integrity." Frontiers in Nutrition 7 (2020): 295.
[4] Mossink, J P. “Zinc as nutritional intervention and prevention measure for COVID-19 disease.” BMJ nutrition, prevention & health vol. 3,1 111-117. 17 Jun. 2020, doi:10.1136/bmjnph-2020-000095
[5] Mayor-Ibarguren, Ander et al. “A Hypothesis for the Possible Role of Zinc in the Immunological Pathways Related to COVID-19 Infection.” Frontiers in immunology vol. 11 1736. 10 Jul. 2020, doi:10.3389/fimmu.2020.01736
[6] Wessels, Inga et al. “The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis.” Frontiers in immunology vol. 11 1712. 10 Jul. 2020, doi:10.3389/fimmu.2020.01712
[vii] Mayor-Ibarguren, Ander et al. “A Hypothesis for the Possible Role of Zinc in the Immunological Pathways Related to COVID-19 Infection.” Frontiers in immunology vol. 11 1736. 10 Jul. 2020, doi:10.3389/fimmu.2020.01736 [R]
[viii] Jothimani, Dinesh et al. “COVID-19: Poor outcomes in patients with zinc deficiency.” International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases vol. 100 (2020): 343-349. doi:10.1016/j.ijid.2020.09.014
[ix] Souza, Ana Carolina Remondi, et al. "Zinc, Vitamin D and Vitamin C: Perspectives for COVID-19 With a Focus on Physical Tissue Barrier Integrity." Frontiers in Nutrition 7 (2020): 295.
[x] Souza, Ana Carolina Remondi, et al. "Zinc, Vitamin D and Vitamin C: Perspectives for COVID-19 With a Focus on Physical Tissue Barrier Integrity." Frontiers in Nutrition 7 (2020): 295.
[xi] Alexander, Jan et al. “Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19.” Nutrients vol. 12,8 2358. 7 Aug. 2020, doi:10.3390/nu12082358
[xii] Souza, Ana Carolina Remondi, et al. "Zinc, Vitamin D and Vitamin C: Perspectives for COVID-19 With a Focus on Physical Tissue Barrier Integrity." Frontiers in Nutrition 7 (2020): 295.
[xiii] Wessels, Inga et al. “The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis.” Frontiers in immunology vol. 11 1712. 10 Jul. 2020, doi:10.3389/fimmu.2020.01712
[xiv] Abdelmaksoud, Aida A et al. “Olfactory Disturbances as Presenting Manifestation Among Egyptian Patients with COVID-19: Possible Role of Zinc.” Biological trace element research, 1–8. 7 Jan. 2021, doi:10.1007/s12011-020-02546-5
[xv] Hess, Sonja Y et al. “Use of serum zinc concentration as an indicator of population zinc status.” Food and nutrition bulletin vol. 28,3 Suppl (2007): S403-29. doi:10.1177/15648265070283S303
[xvi] Lozada-Nur, Francina et al. “Dysgeusia in COVID-19: Possible Mechanisms and Implications.” Oral surgery, oral medicine, oral pathology and oral radiology vol. 130,3 (2020): 344-346. doi:10.1016/j.oooo.2020.06.016
[xvii] Ray, Chinmaya Sundar, et al. "Low alkaline phosphatase (ALP) in adult population an indicator of zinc (Zn) and magnesium (Mg) deficiency." Current Research in Nutrition and Food Science Journal 5.3 (2017): 347-352. doi : http://dx.doi.org/10.12944/CRNFSJ.5.3.20
[xviii] Quest Diagnostics. Zinc and RBC zinc.
[xix] Labcorp Zinc.






