Albumin is All Bummin' in COVID-19
Dicken Weatherby, N.D. and Beth Ellen DiLuglio, MS, RDN, LDN
Albumin is a key visceral protein that maintains capillary oncotic pressure and serves as a carrier for hormones, minerals, and fatty acids. It is a negative acute-phase protein, therefore variations in serum levels are dependent on clinical status.[I]
The ODX COVID-19 Series
- COVID-19: The pandemic that has become endemic
- COVID-19: Overlapping risk factors and chronic disease
- Nutritional status
COVID-19: A covert factor in disease susceptibility - COVID-19: Blood chemistry biomarker patterns - Clues and patterns lurking just under the surface
- COVID-19: Blood chemistry biomarker patterns - Down the research rabbit hole
- COVID-19: Blood Biomarkers - Neutrophils
- COVID-19: Blood Biomarkers - Albumin
- COVID-19: BloodBiomarkers - Cytokines
- COVID-19: Blood Biomarkers - Interleukin-6
- COVID-19: Blood Biomarkers - Interleukin-10
- COVID-19: Blood Biomarkers - Vitamin C
- COVID-19: Blood Biomarkers - Vitamin D
- COVID-19: Blood Biomarkers - Zinc
- Biomarker characteristics and blood type - help sharpen the COVID-19 clinical picture
- COVID-19: Initial indications and conventional interventions
- COVID-19: Long-term risk reduction - Naturopathic, functional medicine, and nutrition-based approaches to prevention
- A healthy diet is primary prevention for COVID-19
- You should have a gut feeling about COVID-19
- Beyond dietary food patterns…plant-based compounds may mitigate COVID-19 risk
- Targeted nutrition support in the battle against COVID-19
- Targeted nutrition support in COVID-19: Armed with vitamin C
- Targeted nutrition support in COVID-19: In sync with zinc
- Targeted nutrition support in COVID-19: Micronutrients and phytonutrients are important players
- Optimal Takeaways for improving immunity and reducing susceptibility to COVID-19
- Optimal - The Podcast: Episode 8 -Blood Biomarkers and Risk Factors for COVID-19 and its Comorbidities
Low serum albumin is associated with critical illness, mortality, inflammation, and disease state (organ dysfunction, pancreatitis, burn, trauma, infection). Decreased levels are likely due to an increase in capillary permeability; decrease in protein synthesis; reduced total mass and half-life of albumin; increased volume distribution; and increased vascular endothelial growth factor expression.[ii] Inflammation, severe chronic malnutrition, malignancy, and fluid overload can also lead to hypoalbuminemia.[iii]
A meta-analysis of 11 studies published through April 3, 2020 revealed that patients with severe COVID-19 had a significantly lower admission albumin (3.5 g/dL) than those with non-severe COVID-19 (4.05 g/dL).[iv]
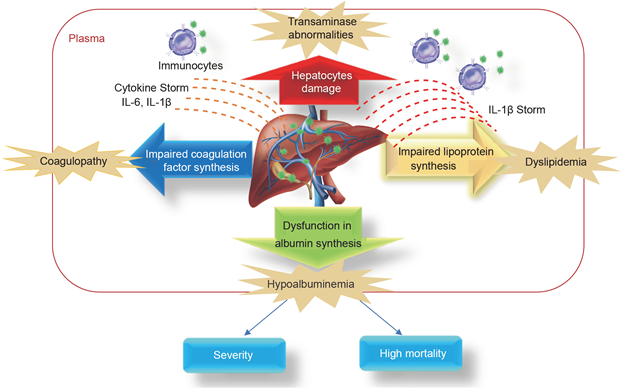
A retrospective study of 2623 adult COVID-19 patients revealed that production and serum levels of albumin, LDL, and HDL decreased with severity of COVID-19.[v]
- Median admission albumin was 3.66 mg/dL in non-critical cases, 3.22 in critical cases, and 3.11 in those who died of COVID-19.
- The second measurement revealed that median albumin significantly decreased: 3.55 in non-critical, 3.13 in critical, and 2.88 in those who died.
- Researchers attribute decreased albumin and lipoprotein synthesis to the negative effects of the cytokine storm characteristic of COVID-19.
COVID-19 patients showed a decline in albumin and lipid synthesis as the severity of the disease developed[vi]
| Biomarker |
Non-critically ill |
Critically ill |
Death |
P |
|
|
ALB (median (IQR)) |
At admission |
36.60 (33.18, 40.40) |
32.20 (29.60, 35.75) |
31.10 (27.85, 34.20) |
<0.001 |
|
Second test |
35.50 (32.40, 38.50) |
31.30 (28.80, 34.52) |
28.80 (25.40, 31.35) |
<0.001 |
|
|
GLO (median (IQR)) |
At admission |
31.70 (28.60, 35.40) |
34.40 (30.55, 38.55) |
36.05 (32.77, 39.20) |
<0.001 |
|
Second test |
31.00 (27.80, 34.30) |
33.00 (29.35, 37.70) |
33.70 (30.70, 38.45) |
<0.001 |
|
|
TP (median (IQR)) |
At admission |
68.70 (65.20, 72.20) |
66.70 (63.10, 70.80) |
67.05 (62.68, 71.03) |
<0.001 |
|
Second test |
66.75 (63.20, 70.23) |
65.10 (60.27, 69.53) |
62.40 (58.30, 67.50) |
<0.001 |
|
|
ALB/GLO (median (IQR)) |
At admission |
1.16 (0.96, 1.38) |
0.93 (0.79, 1.10) |
0.84 (0.74, 0.98) |
0.558 |
|
Second test |
1.15 (0.97, 1.34) |
0.94 (0.79, 1.10) |
0.84 (0.71, 0.98) |
<0.001 |
|
|
TG (median (IQR)) |
At admission |
1.25 (0.96, 1.77) |
1.30 (0.99, 1.71) |
1.55 (1.18, 2.21) |
<0.001 |
|
Second test |
1.48 (1.09, 2.10) |
1.48 (1.07, 2.02) |
1.69 (1.25, 2.31) |
<0.001 |
|
|
HDL-C (median (IQR)) |
At admission |
0.95 (0.80, 1.16) |
0.86 (0.73, 1.05) |
0.77 (0.56, 0.92) |
<0.001 |
|
Second test |
0.99 (0.83, 1.20) |
0.92 (0.74, 1.12) |
0.72 (0.56, 0.87) |
<0.001 |
|
|
LDL-C (median (IQR)) |
Second test |
2.44 (1.96, 2.97) |
2.09 (1.60, 2.68) |
1.92 (1.43, 2.52) |
<0.001 |
|
Second test |
2.50 (2.02, 2.95) |
2.29 (1.68, 2.83) |
1.84 (1.36, 2.47) |
<0.001 |
|
Data are shown as median (IQR). P values were calculated by Kruskal-Wallis rank-sum test. The plasma levels of albumin (ALB), globulin (GLO), total protein (TP), and ALB/GLO were included as serum protein and triglyceride (TG), cholesterol (TC), HDL-C, and LDL-C levels upon admission and after admission. P values were compared among non-critically ill, critically ill, and death groups. If the values of biomarkers were below the lower reference limit, half of the lower reference value was used.
Source: Huang, Wei et al. “Decreased serum albumin level indicates poor prognosis of COVID-19 patients: hepatic injury analysis from 2,623 hospitalized cases.” Science China. Life sciences vol. 63,11 (2020): 1678-1687. Doi:10.1007/s11427-020-1733-4 This article is made available via the PMC Open Access Subset for unrestricted research re-use and secondary analysis in any form or by any means with acknowledgment of the original source. These permissions are granted for the duration of the World Health Organization (WHO) declaration of COVID-19 as a global pandemic.
Serum albumin was significantly lower in non-survivors (3.05 g/dL) versus survivors (3.76 g/dL) in a cohort of 299 adult COVID-19 patients. Albumin correlated inversely with total white blood cells count and neutrophil to lymphocyte ratio in these patients. Ultimately, in this cohort, hypoalbuminemia, lymphopenia, and co-morbidities were independently predictive of mortality.[vii]
Another retrospective study of 134 COVID-19 patients revealed a significant difference in serum albumin between non-survivors (3.35 g/dL) and survivors (3.92 g/dL).[viii]
Hypoalbuminemia associated with COVID-19 may be due to systemic inflammation which increases capillary permeability resulting in migration of albumin into interstitial spaces.[ix]
Standard reference range albumin
Quest[x] 3.6-5.1 g/dL
Labcorp[xi] ~3.9-5.2 g/dL
ODX Optimal 4.0 - 5.0 g/dl
Ratio of Fibrinogen to Albumin (FAR)
The FAR value increases with severe infection and malignancy and is considered a marker of inflammation.
In a retrospective analysis of 113 patients, an elevated ratio of fibrinogen to albumin was considered an independent risk factor for predicting the severity of COVID-19.[xii] An optimal cut-off for FAR was 0.0883 or greater for severe COVID-19. The analysis also found that a platelet count of 135*109/L or less was an independent predictor of severe disease.
Although a variety of factors can influence albumin synthesis and circulating levels, it is still an important tool in the assessment of the clinical status of COVID-19 patients.
Next Up - COVID-19: Blood Biomarkers - Cytokines
Research
[i] Bharadwaj, Shishira et al. “Malnutrition: laboratory markers vs nutritional assessment.” Gastroenterology report vol. 4,4 (2016): 272-280. doi:10.1093/gastro/gow013
[ii] Aziz, Muhammad et al. “The association of low serum albumin level with severe COVID-19: a systematic review and meta-analysis.” Critical care (London, England) vol. 24,1 255. 26 May. 2020, doi:10.1186/s13054-020-02995-3
[iii] Keller, Ulrich. “Nutritional Laboratory Markers in Malnutrition.” Journal of clinical medicine vol. 8,6 775. 31 May. 2019, doi:10.3390/jcm8060775
[iv] Aziz, Muhammad et al. “The association of low serum albumin level with severe COVID-19: a systematic review and meta-analysis.” Critical care (London, England) vol. 24,1 255. 26 May. 2020, doi:10.1186/s13054-020-02995-3
[v] Huang, Wei et al. “Decreased serum albumin level indicates poor prognosis of COVID-19 patients: hepatic injury analysis from 2,623 hospitalized cases.” Science China. Life sciences vol. 63,11 (2020): 1678-1687. doi:10.1007/s11427-020-1733-4
[vi] Huang, Wei et al. “Decreased serum albumin level indicates poor prognosis of COVID-19 patients: hepatic injury analysis from 2,623 hospitalized cases.” Science China. Life sciences vol. 63,11 (2020): 1678-1687. doi:10.1007/s11427-020-1733-4
[vii] Huang, Jiaofeng et al. “Hypoalbuminemia predicts the outcome of COVID-19 independent of age and co-morbidity.” Journal of medical virology, 10.1002/jmv.26003. 14 May. 2020, doi:10.1002/jmv.26003
[viii] Li, Juyi et al. “Plasma albumin levels predict risk for nonsurvivors in critically ill patients with COVID-19.” Biomarkers in medicine vol. 14,10 (2020): 827-837. doi:10.2217/bmm-2020-0254
[ix] Huang, Wei et al. “Decreased serum albumin level indicates poor prognosis of COVID-19 patients: hepatic injury analysis from 2,623 hospitalized cases.” Science China. Life sciences vol. 63,11 (2020): 1678-1687. doi:10.1007/s11427-020-1733-4
[x] Quest Diagnostics Albumin - https://testdirectory.questdiagnostics.com/test/test-detail/223/albumin?cc=MASTER
[xi] Labcorp Albumin - https://www.labcorp.com/tests/001081/albumin
[xii] Bi, Xiaojie et al. “Prediction of severe illness due to COVID-19 based on an analysis of initial Fibrinogen to Albumin Ratio and Platelet count.” Platelets vol. 31,5 (2020): 674-679. doi:10.1080/09537104.2020.1760230






