Welcome to part 8 of the ODX Andropause & Low T Syndrome Series. Lifestyle factors play a role in the etiology and resolution of LOH, just as they play a role in some of the metabolic disorders that contribute to LO, including type 2 diabetes and obesity.[1]
The ODX Male Andropause Series
- Andropause Part 1 – An Introduction
- Andropause Part 2 – Biology & Physiology
- Andropause Part 3 – How to identify it
- Andropause Part 4 – Lab Assessment and Biomarker Guideposts
- Andropause Part 5 – Clinical Determination
- Andropause Part 6 – Lab Reference Ranges
- Andropause Part 7 – How do we treat and counteract andropause?
- Andropause Part 8 – Lifestyle approaches to addressing Andropause
- Andropause Part 9 – Optimal Takeaways
- Optimal The Podcast – Episode 9: Andropause
Ideally, lifestyle improvements and weight loss when needed should precede testosterone therapy which then can be initiated in those with persistently low T.[2]
Lifestyle modifications are recommended for LOH individuals with obesity, metabolic syndrome, and type 2 diabetes.[3] Primary modifications include increased physical activity and maintaining a healthy diet and a healthy weight.
Chronic lifestyle-related diseases, including cardiovascular disease, T2DM, and excess inflammation, increase risk of LOH by a factor of 1.5-3.6. A BMI of 30 or greater increases risk of LOH by a factor of 13.[4] Implementing lifestyle changes to address each of these related comorbidities would be most prudent. [5]
The Diabetes Prevention Program revealed that intensive lifestyle changes were effective in promoting weight loss and increased TT levels when compared to placebo or metformin intervention in men with a mean BMI of 32. Weight loss after 12 months in the lifestyle group was 7.87 kg and TT levels increased by 33 ng/dL (1.15 nmol/L) with no changes in T in the placebo or metformin groups.[6]
It is possible to increase endogenous production of testosterone with healthy lifestyle choices, treatment of sleep apnea, discontinuation of interfering medications (e.g., opioids, carbamazepine), and weight loss.
Although the International Society for Sexual Medicine (ISSM) does recommend non-pharmacological intervention for LOH, they also recognize that individual compliance can be low and T therapy may be indicated.[7]
Committing the LEMON mnemonic to memory can remind practitioners to complete a full evaluation before setting out on the best course for each individual.[8]
- L Lifestyle
- E Endocrine
- M Medical/metabolic
- O Observer-induced/iatrogenic
- N Nutritional
Diet and nutrition
An unhealthy diet, such as the Western diet high in processed foods and low in fruits, vegetables, whole grains, and fish, can have negative effects on men’s sexual health and possibly fertility.[9]
A healthy foundation replete in unprocessed foods, fruits, vegetables, legumes, whole grains, nuts, seeds, herbs, spices, and high quality fats and protein can help maintain a healthy weight and reduce the risk of metabolic disorders that contribute to LOH.
In one pilot study of male obesity secondary hypogonadism (MOSH) individuals with TT below 349 ng/dL (12.1 nmol/L), a balanced Mediterranean-style diet significantly increased TT within 2-4 months. Characteristics of the approach included:[10] [11]
- An abundance of fresh vegetables, fruit, extra virgin olive oil, protein, fish, legumes, grains
- A 170-250 kcal/d reduction from basal metabolic needs
- Protein 1.5 grams/kg ideal body weight
- 45-50% carbohydrate
- 30% fat
- 25-30 grams of fiber/day
- Less than 5 grams of sodium/day
- No alcohol
- Physical activity 150 minutes/week of mild intensity aerobic activity and/or 90 minutes high intensity activity at least 3 days per week.
- Goal was 10% reduction in weight from baseline
Micronutrient status is important to hormonal balance as well. Micronutrients being studied for their roles in testosterone metabolism include zinc, magnesium, boron, vitamin C, vitamin D, D-aspartic acid, and conjugated linoleic acid.[12] It remains practical to ensure that micronutrient status in those with LOH and its comorbidities, especially when micronutrient insufficiency is present.
A small study indicated that consumption of an organic diet was significantly associated with improvements in Sexual Health Inventory for Men (SHIM) scores before adjusting for age and BMI. In those following an organic diet, hypogonadism was diagnosed in 3.3% versus 15.7% in those who did not. Intermittent fasting was also assessed in the study with 6.5% being diagnosed with hypogonadism versus 15.5% of those who did not apply intermittent fasting.[13]
Environmental toxins such as pesticides, phthalates, chlorinated pollutants, and other xenobiotics can act as endocrine disruptors, reduce testosterone, and contribute to hypogonadism and infertility.[14] [15] Exposure to them in the diet and the environment can have detrimental effects on health and hormone balance.
Weight loss
It is generally accepted that most secondary hypogonadism caused by obesity can be reversed with weight loss. Indeed, weight loss in this population is considered first line therapy as the combination of low T and abdominal obesity may predict increased mortality risk.[16]
An interesting phenomenon occurs in obese hypogonadal men with insulin resistance. Elevated insulin inhibits SHBG secretion from the liver leading to a temporary increase in free T which can then be aromatized to estradiol in adipose tissue. This can create a negative feedback for the hypothalamic-pituitary-testicular axis. The inflammatory nature of obesity can also affect testosterone metabolism and contribute to hypogonadism. Research suggests that a weight loss of at least 10% be achieved in order to significantly increase circulating T and improve symptoms.[17]
The EMAS study established that weight gain and increased waist circumference can lead to a decrease in total and free T. Fortunately it also indicated that weight loss can increase both measurements, making weight and obesity a modifiable risk factor in LOH.[18]
A prospective follow up study of EMAS participants revealed that weight loss of 5% or more in obese men with LOH was found to improve serum T levels from 265 ng/dL (9.2 nmol/L) to 383 ng/dl (13.3 nmol/L). However, symptoms were not significantly improved in these individuals. Researchers note that these biochemical improvements were not as dramatic as with T therapy which can yield a 2-fold increase in serum T into the mid-normal physiological range in a 24-week period. Randomized controlled research also demonstrates improvements in physical strength, sexual function, and symptoms of depression with T therapy.[19]
Exercise
Exercise can improve T levels:[20]
- Acute exercise in conditioned individuals can induce significant increases in serum testosterone from pre- to post-exercise period.
- Moderate intensity resistance exercise induced an increase in young and middle-aged men.
- Exercise can increase growth hormone
A 12-week lifestyle modification program for overweight and obese men was associated with significantly increased T with a subsequent significant decrease in central blood pressure. Intervention and results included:[21]
- Calorie restricted diet ~1680 Kcals/day with balanced macronutrients (50% carbs, 25% protein, 25% fat) and nutrition education regarding a healthy diet, vitamins, and minerals.
- Aerobic exercise incorporating walking or jogging 40-60 minutes three times per week
- Total and LDL cholesterol, triglycerides, and insulin decreased significantly
- Serum TT increased from a mean of 355 to 380 ng/dL (12.3 to 13.2 nmol/L) respectively
Plant-based compounds
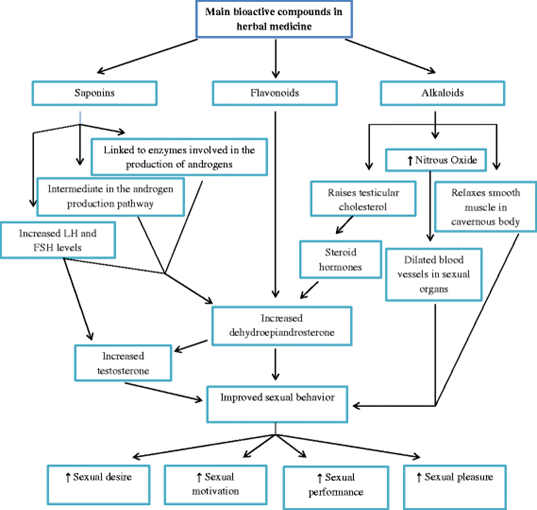
Plants are complex chemical factories, and many phytochemicals exert effects on testosterone levels via a variety of mechanisms, including modulation of gene expression.
Phytochemicals that appear to support testosterone metabolism include flavonoids apigenin, chrysin, luteolin, and quercetin. At the cellular level, these phytochemicals appear to promote entry of cholesterol into the mitochondria of testicular Leydig cells where increased testosterone production can take place. Some phytochemicals, including chrysin and apigenin, inhibit aromatase and conversion of testosterone to estradiol.
Food sources include: [22]
- Anthocyanidins found in berries, currants, grapes, tea, tropical fruits, and wine
- Apigenin and luteolin flavones found in celery, parsley, and thyme
- Catechin flavonoids found in apples, red wine, and tea
- Chrysin flavonoids found in chamomile, fruit bark, honey, mushrooms, propolis, and other plant extracts
- Naringenin and hesperidin flavanones found in citrus and plums
- Quercetin, myricetin, and kaempferol flavonols found in apples, berries, broccoli, cherries, onions, and tea
Adequate endogenous levels of relevant phytochemicals can be achieved with a robust intake of fresh fruits and vegetables. Also note that many phytochemicals and antioxidants increase in produce as it ripens so crops should be harvested accordingly.[23] [24]
Medicinal plants
Many plant-based herbal compounds have been studied for their effects on testosterone and symptoms of LOH. Although many have been used in traditional medicine throughout time, existing research may be limited or primarily conducted on animals. Researchers recommend more in depth high quality studies before drawing conclusions in a 2014 review:[25]
- Astragalus root (Astragalus membranaceus) (limited research)
- Barrenwort (herba epimedium) (warrants further research)
- Chinese yam (limited research)
- Fenugreek (Trigonella foenum-graecum) (ongoing research)
- Ginkgo biloba (warrants further research)
- Ginseng
- Longjack root (eurycoma longifolia) (ongoing research)
- One month supplementation with 200 mg standardized extract highly significantly increased serum T in LOH subjects from a mean of 163 to 240 to ng/dL (5.66 to 8.31 nmol/L) and highly significantly improved symptoms.[26]
- Passionflower (Passiflora incarnate) (ongoing research)
- Tribulus terrestris (ongoing research)
- Velvet bean extract (mucuna pruriens) (warrants further research)
In China, Malaysia, and Indonesia, several plant-based compounds have been used traditionally to improve testosterone metabolism by facilitating its release from binding globulins or enhancing receptor engagement. Though researchers encourage more stringent evaluation via controlled studies, the following compounds have been used traditionally with positive results:[27]
- Ashwaganda
- Epimedium Extract (Horny Goat Weed)
- Ginseng (Panax Ginseng)
- Lunasia amara Blanco ( Sanrego )
- Muira Puama (Ptychopetalum olacoides)
- Nettle leaf
- Pimpinella alpina ( Purwoceng )
- Pumpkin seed
- Pygeium
- Rye grass
- Saw palmetto
- Tongkat Ali (Eurycoma longifolia)
- Tribulus terrestris
- Wild oats, Avena sativa
The plant-based compound Trigonella foenum-graecum seed extract (fenugreek) was tested via a double-blind placebo-controlled study of 120 males with symptoms of androgen deficiency aged 43-75. Results demonstrated a significant decrease in symptoms determined by the Aging Male Symptoms Questionnaire. Sexual health and serum testosterone also increased after the 12-week treatment period. In this study:[28]
- Serum testosterone in the treatment group increased significantly from a mean of 355 ng/dL to 398 ng/dL, 12.3 to 13.8 nmol/L respectively.
- Free testosterone increased from a mean of 69.4 pg/mL (241 pmol/L) to 76 pg/mL (264 pmol/L).
- Treatment was well tolerated.
- Total sexual function score increased in the active group from 66.2 at baseline to 76.3 at week 12; the score in the placebo group went from a baseline of 57.8 to 57 at week 12.
Animal studies reveal a number of food components and supplements that positively impact T levels and may have applications in humans pending further research. The main mechanisms observed were:[29]
- Promotion of T-production, including regulation of LH ( which stimulates T production) and testosterone synthase (which synthesizes T)
- Inhibiting enzymes that degrade T
- Alleviating testicular toxicity and T suppression, especially via antioxidant activity
Actions of food components on T metabolism ( - = no data)
Promoting T-production / Inhibiting T-degradation / Alleviating testicular toxicity
- Garlic + - +
- Ginger + - -
- Lactic acid bacteria + - +
- Soybeans + - +
- Amino acid + - +
- L-arginine + - +
- L-carnitine + - +
- Linoleic Acid + - -
- Selenium + - +
- Vitamin (C/E) + - +
- Zinc + - +
- Beta-caryophyllene - + -
- Chrysin - + -
- Coenzyme Q10 + - +
- Cordyceps Militaris + - -
- Curcumin - - +
- Cuscuta chinensis - - +
- Emu oil - - +
- Fish oil + - -
- Fucoxanthin + - -
- Geranylgeraniol + - -
- Guarana + - +
- Hazelnut + (Aged only) - -
- Lutein - - +
- Maca + - +
- Melatonin + - +
- Milk thistle seed and rosemary leaf + - -
- Moringa + - +
- N-acetyl-cysteine - - +
- Oleuropein + - -
- Piperine + - -
- Propolis and Royal Jelly + - +
- Resveratrol + - +
- Rooibos + - -
- Saccharomyces cerevisiae + - -
- Taxifolin - - +
Source: Kataoka, Tomoya, Yuji Hotta, and Kazunori Kimura. "A Review of foods and food supplements increasing testosterone levels." (2021). This is an open-access article under the CC BY 4.0 license ()
Herbal medicine mechanisms of action[xxx]
|
Intervention |
Gender (n) |
Action mechanism |
|
T. terrestris |
M (30) |
A saponin that acts in the erectile function, when converted into Dehydroepiandrosterone (DHEA), which acts on ↑ intracavernous pressure. |
|
E. longifolia |
M (109) |
↑ Testosterone → range of bioactive phenolic compounds: polypeptides, diterpenoids, alkaloids, quassinoids, and others. |
|
Low-energy diet and low-fat, high-protein diet |
M (31) |
Diet ↑ testosterone and improves sexual function. |
|
Maca root |
F (17) M (3) |
Effect on serum levels of gonadal hormone, LH, FSH, PRL, 17-alpha hydroxyprogesterone, TST, and 17-beta-estradiol. |
|
Vigodana supplement consisting of Rhodiola rosea combined with vitamins and minerals |
F (83) M (37) |
Influences the metabolism of neurotransmitters, such as serotonin, dopamine, noradrenalin, acetylcholine; ↑ permeability of the hematoencephalic barrier. |
|
Essential phospholipids |
M (23) |
↓ Number of patients with erectile dysfunction and loss of libido. ↑ Number and motility of spermatozoids and ↑ activity of enzymes involved in lipidic metabolism. |
|
Alcohol |
F/M (17000) |
↑ Sexual excitement; ↓ sexual function, reproduction, performance, ejaculatory capacity, insemination, masculine hormones, and spermatogenesis. May also cause infertility. |
|
Zinc sulfate |
M (8) |
Important in biosynthesis of RNA and DNA. Improves testicular function ↑ plasmatic testosterone, and ↑ FSH. |
F female, M male
Adapted from da Cruz, Amanda Cássia, et al. "The action of herbal medicine on the libido: aspects of nutritional intervention in increasing sexual desire." Nutrire 42.1 (2017): 1-8. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (), Does not include exclusively female research.
Source: da Cruz, Amanda Cássia, et al. "The action of herbal medicine on the libido: aspects of nutritional intervention in increasing sexual desire." Nutrire 42.1 (2017): 1-8. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License
Optimal Takeaways for lifestyle, nutrition, and naturopathic approaches to Andropause / Low T syndrome / LOH
Remember the LEMON mnemonic when evaluating dysfunction:
- L Lifestyle
- E Endocrine
- M Medical/metabolic
- O Observer-induced/iatrogenic
- N Nutritional
Important lifestyle modifications that support healthy testosterone metabolism include:
- A healthy balanced Mediterranean-style diet that includes an abundance of vegetables, fruits, whole grains, legumes, nuts, seeds, herbs, spices, and fish, organic as available.
- Regular activity including 90-150 minutes of mild to moderate intensity exercise at least 3 days per week.
- Weight loss of at least 10% in obese men with LOH
- Micronutrient sufficiency, supplementation as needed
- Some plant-based compounds and herbs may have beneficial effects on T levels though additional research is indicated. The most promising compounds include
- Longjack root (eurycoma longifolia)
- Fenugreek seed extract (trigonella foenum-graecum)
- Tribulus terrestris
NEXT UP: Andropause Part 9 –Optimal Takeaways
Research
[1] Braga, Patrícia C et al. “Late-onset hypogonadism and lifestyle-related metabolic disorders.” Andrology vol. 8,6 (2020): 1530-1538. doi:10.1111/andr.12765
[2] Giagulli, Vito Angelo et al. “Critical evaluation of different available guidelines for late-onset hypogonadism.” Andrology vol. 8,6 (2020): 1628-1641. doi:10.1111/andr.12850
[3] Singh, Parminder. “Andropause: Current concepts.” Indian journal of endocrinology and metabolism vol. 17,Suppl 3 (2013): S621-9. doi:10.4103/2230-8210.123552.
[4] Swee, Du Soon, and Earn H Gan. “Late-Onset Hypogonadism as Primary Testicular Failure.” Frontiers in endocrinology vol. 10 372. 12 Jun. 2019, doi:10.3389/fendo.2019.00372
[5] Huhtaniemi, Ilpo. “Late-onset hypogonadism: current concepts and controversies of pathogenesis, diagnosis and treatment.” Asian journal of andrology vol. 16,2 (2014): 192-202. doi:10.4103/1008-682X.122336
[6] Giagulli, Vito Angelo et al. “The Role of Diet and Weight Loss in Improving Secondary Hypogonadism in Men with Obesity with or without Type 2 Diabetes Mellitus.” Nutrients vol. 11,12 2975. 5 Dec. 2019, doi:10.3390/nu11122975
[7] Lawrence, Kristi L et al. “Approaches to male hypogonadism in primary care.” The Nurse practitioner vol. 42,2 (2017): 32-37. doi:10.1097/01.NPR.0000511774.51873.da
[8] Kalra, Sanjay et al. “Management of late-onset hypogonadism: person-centred thresholds, targets, techniques and tools.” The journal of the Royal College of Physicians of Edinburgh vol. 51,1 (2021): 79-84. doi:10.4997/JRCPE.2021.121
[9] La, Justin et al. “Diet and Men's Sexual Health.” Sexual medicine reviews vol. 6,1 (2018): 54-68. doi:10.1016/j.sxmr.2017.07.004
[10] Giagulli, Vito Angelo et al. “The Role of Diet and Weight Loss in Improving Secondary Hypogonadism in Men with Obesity with or without Type 2 Diabetes Mellitus.” Nutrients vol. 11,12 2975. 5 Dec. 2019, doi:10.3390/nu11122975
[11] De Lorenzo, Antonino et al. “MOSH Syndrome (Male Obesity Secondary Hypogonadism): Clinical Assessment and Possible Therapeutic Approaches.” Nutrients vol. 10,4 474. 12 Apr. 2018, doi:10.3390/nu10040474
[12] Gunnels, Trint A., and Richard J. Bloomer. "Increasing circulating testosterone: impact of herbal dietary supplements." Journal of Plant Biochemistry & Physiology (2014).
[13] El-Khatib, Farouk M., et al. "Adherence to an Organic Diet is Protective Against Hypogonadism and Erectile Dysfunction." JOURNAL OF SEXUAL MEDICINE. Vol. 17. No. 1. THE BOULEVARD, LANGFORD LANE, KIDLINGTON, OXFORD OX5 1GB, OXON, ENGLAND: ELSEVIER SCI LTD, 2020.
[14] La Nasa Jr, Joseph A. "Obesity, Hypogonadism, and Male Fertility—The Role of Diet and Environment." Bioenvironmental Issues Affecting Men's Reproductive and Sexual Health. Academic Press, 2018. 107-119.
[15] Da Ros, Carlos T., and Túlio M. Graziottin. "Environmental Issues Resulting in Hypogonadism in Brazilian Men." Bioenvironmental Issues Affecting Men's Reproductive and Sexual Health. Academic Press, 2018. 33-40.
[16] Grossmann, Mathis. “Hypogonadism and male obesity: Focus on unresolved questions.” Clinical endocrinology vol. 89,1 (2018): 11-21. doi:10.1111/cen.13723
[17] Giagulli, Vito Angelo et al. “The Role of Diet and Weight Loss in Improving Secondary Hypogonadism in Men with Obesity with or without Type 2 Diabetes Mellitus.” Nutrients vol. 11,12 2975. 5 Dec. 2019, doi:10.3390/nu11122975
[18] Decaroli, Maria Chiara, and Vincenzo Rochira. “Aging and sex hormones in males.” Virulence vol. 8,5 (2017): 545-570. doi:10.1080/21505594.2016.1259053
[19] Rastrelli, Giulia et al. “Development of and Recovery from Secondary Hypogonadism in Aging Men: Prospective Results from the EMAS.” The Journal of clinical endocrinology and metabolism vol. 100,8 (2015): 3172-82. doi:10.1210/jc.2015-1571
[20] Gunnels, Trint A., and Richard J. Bloomer. "Increasing circulating testosterone: impact of herbal dietary supplements." Journal of Plant Biochemistry & Physiology (2014).
[21] Kumagai, Hiroshi et al. “Lifestyle modification increases serum testosterone level and decrease central blood pressure in overweight and obese men.” Endocrine journal vol. 62,5 (2015): 423-30. doi:10.1507/endocrj.EJ14-0555
[22] Martin, Luc J, and Mohamed Touaibia. “Improvement of Testicular Steroidogenesis Using Flavonoids and Isoflavonoids for Prevention of Late-Onset Male Hypogonadism.” Antioxidants (Basel, Switzerland) vol. 9,3 237. 13 Mar. 2020, doi:10.3390/antiox9030237 This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ().
[23] Bhandari, Shiva Ram, and Jun Gu Lee. “Ripening-Dependent Changes in Antioxidants, Color Attributes, and Antioxidant Activity of Seven Tomato (Solanum lycopersicum L.) Cultivars.” Journal of analytical methods in chemistry vol. 2016 (2016): 5498618. doi:10.1155/2016/5498618
[24] Zhou, Yucheng et al. “Accumulation of Anthocyanins and Other Phytochemicals in American Elderberry Cultivars during Fruit Ripening and its Impact on Color Expression.” Plants (Basel, Switzerland) vol. 9,12 1721. 7 Dec. 2020, doi:10.3390/plants9121721
[25] Gunnels, Trint A., and Richard J. Bloomer. "Increasing circulating testosterone: impact of herbal dietary supplements." Journal of Plant Biochemistry & Physiology (2014).
[26] Tambi, M I B M et al. “Standardised water-soluble extract of Eurycoma longifolia, Tongkat ali, as testosterone booster for managing men with late-onset hypogonadism?.” Andrologia vol. 44 Suppl 1 (2012): 226-30. doi:10.1111/j.1439-0272.2011.01168.x
[27] Lim, Peter Huat Chye. "Traditional Asian Herbs: Potential Use for Late-Onset Hypogonadism?." Men's Health. Springer, London, 2013. 77-82.
[28] Rao, Amanda et al. “Testofen, a specialised Trigonella foenum-graecum seed extract reduces age-related symptoms of androgen decrease, increases testosterone levels and improves sexual function in healthy aging males in a double-blind randomised clinical study.” The aging male : the official journal of the International Society for the Study of the Aging Male vol. 19,2 (2016): 134-42. doi:10.3109/13685538.2015.1135323
[29] Kataoka, Tomoya, Yuji Hotta, and Kazunori Kimura. "A Review of foods and food supplements increasing testosterone levels." (2021). This is an open access article under the CC BY 4.0 license ()
[xxx] da Cruz, Amanda Cássia, et al. "The action of herbal medicine on the libido: aspects of nutritional intervention in increasing sexual desire." Nutrire 42.1 (2017): 1-8. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (),






