Welcome to part 10 of the ODX Stress Biomarkers Series. This post focuses on some of the foods and nutrients that can support a healthy stress response.
The stress response ultimately requires macronutrients and micronutrients to sustain it. This is an especially important time to consume nutrient-dense foods and minimize highly processed foods, especially those high in excess sugar and trans fats. Unfortunately, many comfort foods fall into the latter category but can be modified to improve their nutrition profile or can be limited to minimize their negative impact.
A healthy diet should be based on fresh unprocessed plant-based foods including fruits, vegetables, whole grains, legumes, nuts, seeds, herbs, and spices. The addition of high-quality sources of protein may include cold-water fish, seafood, organic meats, eggs, and dairy. High quality sources of fat include extra virgin olive oil, olives, avocado, flax seeds, chia seeds, hemp seeds, and nuts. Foods should be minimally processed in order to maximize nutrition density; while processed and deep-fried foods should be eliminated or minimized.
Essential oils are plant-based compounds that have been used therapeutically for millennia. They can be concentrated and applied topically or taken in though inhalation, which is one of the most common modes. Essential oils that have a positive modulating effect on stress include cedarwood, clary sage, chamomile, ginseng, lavender, jasmine, neroli, rose, sandalwood, Siberian ginseng, vetiver, ylang ylang.[vii] [viii] [ix] [x] [xi]
Ascorbic acid, more commonly known as vitamin C, plays a role in regulation of the stress response. Vitamin C is stored to some extent in the adrenal gland and is released when cortisol levels increase. The increase in circulating vitamin C is able to “put the brakes” on hyperactivation of the HPA axis.
Vitamin C also acts as a neuromodulator and may have an antidepressant effect. Supplementation was found to improve depressive symptoms and reduce psychological stress in hospitalized patients. Even increasing consumption of vitamin C containing foods such as kiwifruit dramatically improved mood disturbances and fatigue in a group of non-smoking male students.[xii] Vitamin C is essential to a healthy stress response as it: [xiii]
Most mammals produce their own vitamin C from glucose-6-phosphate in the liver. However, humans have lost the ability to do so and are completely dependent on dietary intake. When under stress, other mammals increase production and release of ascorbic acid which supports hemodynamic reserve, immune function, and protection from oxidative stress. For example, a goat produces an estimated 2-4 grams of vitamin C under normal conditions. However, production increases significantly under stress. Without this flexible ability to synthesize vitamin C, humans have an impaired response to stress. Insufficiency of vitamin C will also impede the myriad functions that vitamin C participates in including antioxidant, anti-inflammatory, immune, anti-thrombotic, and adrenergic functions. Vitamin C is also essential to catecholamine synthesis, wound healing, and microcirculation.[xiv]
In one randomized double-blind, placebo-controlled study, supplementation with 3,000 mg/day of sustained-release vitamin C effectively reduced blood pressure and subjective response to acute psychological stress. Supplementation also facilitated a faster normalization of blood pressure and salivary cortisol. The improvement in systolic blood pressure was superior to that achieved with beta-blocker antihypertensives. Plasma vitamin C increased significantly from a baseline mean of 1.55 mg/dL (88 umol/L) to 2.65 mg/dL (150.5 umol/L) in subjects taking vitamin C.[xv]
The gut-brain axis plays a role in regulating the stress response, and resident microbiota participate as well in what is known as the microbiota-gut-brain axis. Ongoing research suggests that the gut microbiota and their optimization through pre- and pro-biotic supplementation may favorably modify the HPA axis, cortisol levels, and an individual’s response to acute and chronic stress.[xvi]
Irritable bowel syndrome (IBS) is a stress-related (or “stress-adjacent”) condition characterized by abdominal pain, visceral sensitivity, and significantly altered gastrointestinal motility. Stress can exacerbate gastrointestinal symptoms and even induce visceral pain in IBS. The gut microbiota may be a factor in the symptomatology and pathophysiology of IBS and its related anxiety and depression. Research suggests that dysbiosis caused by antibiotics can predispose an individual to a heightened sensitivity to visceral pain and may contribute to IBS directly. Supporting and restoring the gut microbiome, i.e., microorganisms, their collective genes, and factors they produce,[xvii] may be therapeutic in IBS though further human studies are needed. Stress may also contribute to increased intestinal permeability or “leaky gut syndrome,” which in turn may contribute to bacterial translocation, inflammation, immune activation, and GI distress.[xviii]
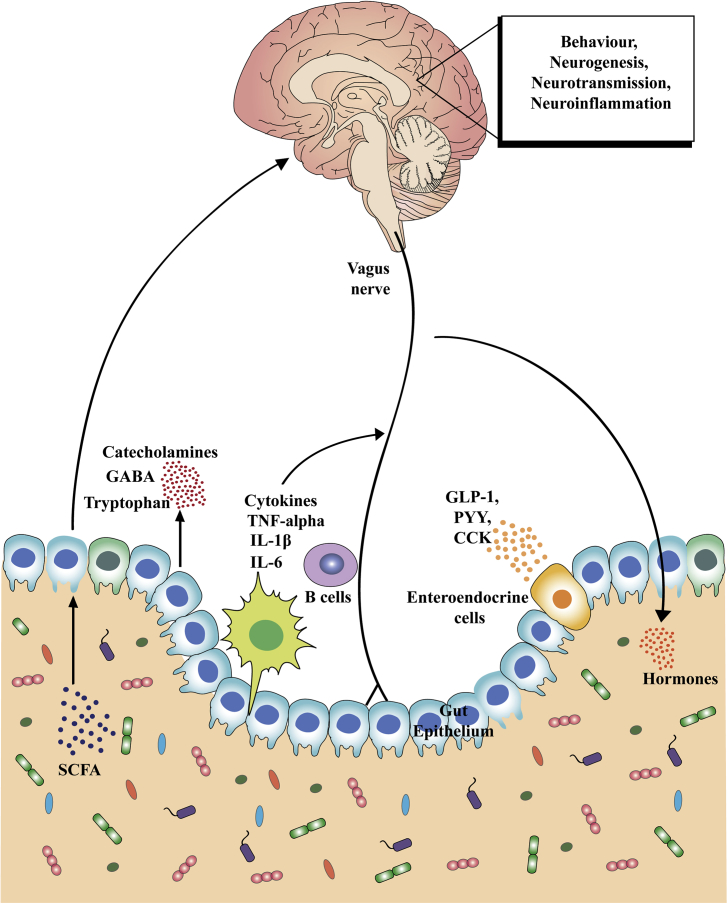
Key communication pathways of the microbiota–gut–brain axis. There are numerous mechanisms through which the gut microbiota can signal to the brain. These include activation of the vagus nerve, production of microbial antigens that recruit immune B cell responses, production of microbial metabolites (i.e. short-chain fatty acids [SCFAs]), and enteroendocrine signaling from gut epithelial cells (e.g., I-cells that release CCK, and L-cells that release GLP-1, PYY and other peptides). Through these routes of communication, the microbiota–gut–brain axis controls central physiological processes, such as neurotransmission, neurogenesis, neuroinflammation and neuroendocrine signaling that are all implicated in stress-related responses. Dysregulation of the gut microbiota subsequently leads to alterations in all of these central processes and potentially contributes to stress-related disorders.
Source: Foster, Jane A et al. “Stress & the gut-brain axis: Regulation by the microbiome.” Neurobiology of stress vol. 7 124-136. 19 Mar. 2017, doi:10.1016/j.ynstr.2017.03.001 This is an open access article under the CC BY-NC-ND license
Early stress, even in utero, can significantly impact the HPA axis and an individual’s ability to mount a healthy response to, and recovery from, stress. Such early stress and associated cortisol elevations can alter the gastrointestinal microbiome, promote dysbiosis, and further exacerbate the impaired response to stress. Research suggests that stress can increase the permeability not only of the GI tract, but of the blood brain barrier (BBB) as well. An increase in BBB permeability can increase neuroinflammation, further amplifying the negative effects of chronic stress.[xix]
The stress-induced dysfunctional relationship created between the gut, the brain, and the microbiota may contribute to mood disorders, behavioral abnormalities, autism, Alzheimer’s, Parkinson’s, brain injury, and stroke.[xx]
Adopting a healthy diet should be integrated into a healthy lifestyle early on so that when highly stressful situations occur, the groundwork is laid to support a quick recovery from acute stress.
[1] Singh, K. "Nutrient and stress management." J Nutr Food Sci 6.4 (2016): 528.
[2] Dhama, Kuldeep et al. “Biomarkers in Stress Related Diseases/Disorders: Diagnostic, Prognostic, and Therapeutic Values.” Frontiers in molecular biosciences vol. 6 91. 18 Oct. 2019, doi:10.3389/fmolb.2019.00091
[3] Geiker, N R W et al. “Does stress influence sleep patterns, food intake, weight gain, abdominal obesity and weight loss interventions and vice versa?.” Obesity reviews : an official journal of the International Association for the Study of Obesity vol. 19,1 (2018): 81-97. doi:10.1111/obr.12603
[4] Murray, Michael T., and Joseph Pizzorno. The encyclopedia of natural medicine third edition. Simon and Schuster, 2012.
[5] Murray, Michael T., and Joseph Pizzorno. The encyclopedia of natural medicine third edition. Simon and Schuster, 2012.
[6] Wardle, Jon, and Jerome Sarris. Clinical naturopathy: an evidence-based guide to practice. Elsevier Health Sciences, 2019. 3rd edition.
[vii] Skidmore-Roth, Linda. Mosby's handbook of herbs & natural supplements. St Louis^ eMO MO: Mosby, 2001.
[viii] Kim, Gyung-Duck, and Soon-Rim Suh. "Meta-analysis about effect of aromatherapy on stress." The Korean journal of hospice and palliative care 11.4 (2008): 188-195.
[ix] Dave, Vivek, and Sachdev Yadav. "Aromatherapy for stress relive." International Journal of Research and Development in Pharmacy and Life Sciences 2 (2013).
[x] Chen, Miao-Chuan et al. “The effects of aromatherapy in relieving symptoms related to job stress among nurses.” International journal of nursing practice vol. 21,1 (2015): 87-93. doi:10.1111/ijn.12229
[xi] Fukumoto, Syuichi, et al. "Effect of flavour components in lemon essential oil on physical or psychological stress." Stress and Health: Journal of the International Society for the Investigation of Stress 24.1 (2008): 3-12.
[xii] Moritz, Bettina et al. “The role of vitamin C in stress-related disorders.” The Journal of nutritional biochemistry vol. 85 (2020): 108459. doi:10.1016/j.jnutbio.2020.108459
[xiii] Moritz, Bettina et al. “The role of vitamin C in stress-related disorders.” The Journal of nutritional biochemistry vol. 85 (2020): 108459. doi:10.1016/j.jnutbio.2020.108459
[xiv] Marik, Paul E. “Vitamin C: an essential "stress hormone" during sepsis.” Journal of thoracic disease vol. 12,Suppl 1 (2020): S84-S88. doi:10.21037/jtd.2019.12.64
[xv] Brody, Stuart et al. “A randomized controlled trial of high dose ascorbic acid for reduction of blood pressure, cortisol, and subjective responses to psychological stress.” Psychopharmacology vol. 159,3 (2002): 319-24. doi:10.1007/s00213-001-0929-6
[xvi] Sherwin, Eoin et al. “May the Force Be With You: The Light and Dark Sides of the Microbiota-Gut-Brain Axis in Neuropsychiatry.” CNS drugs vol. 30,11 (2016): 1019-1041. doi:10.1007/s40263-016-0370-3
[xvii] Tetel, M J et al. “Steroids, stress and the gut microbiome-brain axis.” Journal of neuroendocrinology vol. 30,2 (2018): 10.1111/jne.12548. doi:10.1111/jne.12548
[xviii] Foster, Jane A et al. “Stress & the gut-brain axis: Regulation by the microbiome.” Neurobiology of stress vol. 7 124-136. 19 Mar. 2017, doi:10.1016/j.ynstr.2017.03.001
[xix] Frankiensztajn, Linoy Mia et al. “The microbiota and the hypothalamus-pituitary-adrenocortical (HPA) axis, implications for anxiety and stress disorders.” Current opinion in neurobiology vol. 62 (2020): 76-82. doi:10.1016/j.conb.2019.12.003
[xx] Tetel, M J et al. “Steroids, stress and the gut microbiome-brain axis.” Journal of neuroendocrinology vol. 30,2 (2018): 10.1111/jne.12548. doi:10.1111/jne.12548