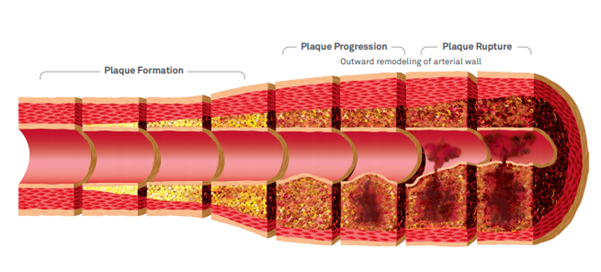
Damage to the endothelium is the first step on the road to full blown atherosclerosis, which contributes to most heart attacks and strokes.[1] Because atherosclerosis causes ischemic heart disease, it is, in fact, considered the main cause of death around the world.
Endothelial dysfunction
Vascular inflammation
Buildup of lipids, cholesterol, calcium, and cellular debris within the intima of the walls of large and medium size arteries
Aging
Antioxidant insufficiency
Chronic inflammation
Elevated homocysteine
Lifestyle factors (sedentary, Western-style diet, obesity, smoking, pollution)
Oxidative stress

Source: Upadhyay, Ravi Kant. “Emerging risk biomarkers in cardiovascular diseases and disorders.” Journal of lipids vol. 2015 (2015): 971453. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continued exposure to cardiovascular risk factors is mirrored in pathological changes to blood vessels. Loss of integrity of the vascular endothelium is accompanied by atherosclerosis, increased smooth muscle cell migration and proliferation, leukocyte migration, and adhesion.[4]
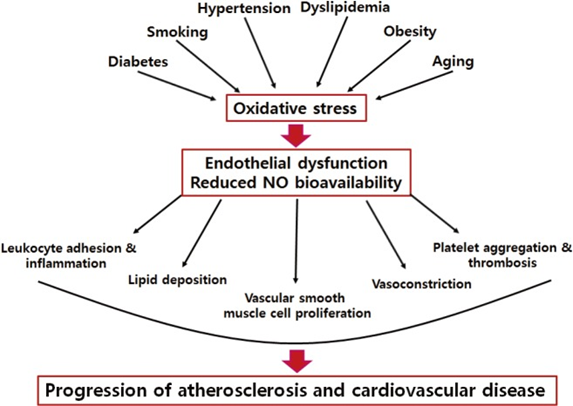
Progression from risk factors to atherosclerosis and cardiovascular disease mediated by oxidative stress and endothelial dysfunction. The early detection of endothelial dysfunction is a critical point in the prevention of atherosclerosis and cardiovascular disease because this dysfunction could be an initial reversible step in the process of atherosclerosis.
Source: Park, Kyoung-Ha, and Woo Jung Park. “Endothelial Dysfunction: Clinical Implications in Cardiovascular Disease and Therapeutic Approaches.” Journal of Korean medical science vol. 30,9 (2015): 1213-25. This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Source: Quest Diagnostics -- https://www.questdiagnostics.com/dms/Documents/Other/CardioIQ_MD46_Brochure.pdf
Early in vivo research demonstrated that atherosclerotic coronary arteries did not dilate in the presence of vasoactive acetylcholine but constricted instead.[5] Endothelial dysfunction continues its rampage even in advanced atherosclerosis as it can promote the rupture of atherosclerotic plaque.[6]
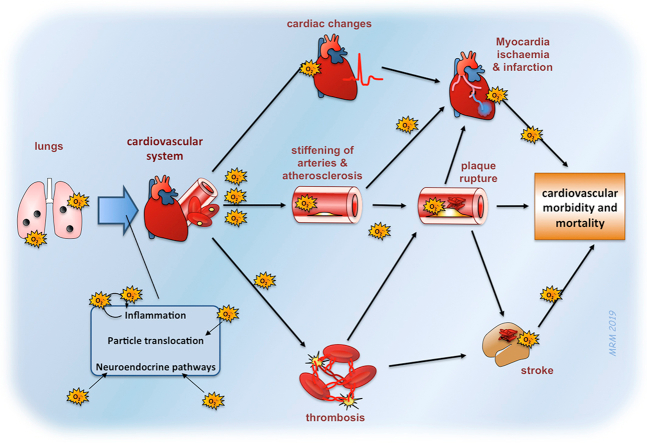
Source: Miller, Mark R. “Oxidative stress and the cardiovascular effects of air pollution.” Free radical biology & medicine vol. 151 (2020): 69-87. This is an open access article under the CC BY license
NEXT UP - Endothelial Dysfunction part 7 - Measuring Endothelial Dysfunction
References[1] Widmer, R Jay, and Amir Lerman. “Endothelial dysfunction and cardiovascular disease.” Global cardiology science & practice vol. 2014,3 291-308. 16 Oct. 2014.
[2] Upadhyay, Ravi Kant. “Emerging risk biomarkers in cardiovascular diseases and disorders.” Journal of lipids vol. 2015 (2015): 971453.
[3] Félétou, Michel. The Endothelium: Part 1: Multiple Functions of the Endothelial Cells—Focus on Endothelium-Derived Vasoactive Mediators. Morgan & Claypool Life Sciences, 2011.
[4] Park, Kyoung-Ha, and Woo Jung Park. “Endothelial Dysfunction: Clinical Implications in Cardiovascular Disease and Therapeutic Approaches.” Journal of Korean medical science vol. 30,9 (2015): 1213-25.
[5] Barthelmes, Jens et al. “Endothelial dysfunction in cardiovascular disease and Flammer syndrome-similarities and differences.” The EPMA journal vol. 8,2 99-109. 6 Jun. 2017.
[6] Barthelmes, Jens et al. “Endothelial dysfunction in cardiovascular disease and Flammer syndrome-similarities and differences.” The EPMA journal vol. 8,2 99-109. 6 Jun. 2017.
[7] Miller, Mark R. “Oxidative stress and the cardiovascular effects of air pollution.” Free radical biology & medicine vol. 151 (2020): 69-87.