Alanine aminotransferase (ALT)) and aspartate aminotransferase (AST) are enzymes that participate in gluconeogenesis by transferring amino groups to alpha-ketoglutaric acid from alanine (to produce pyruvic acid) or from aspartic acid (to produce oxaloacetic acid). They are often called “liver enzymes” though they are found in other tissues.
ALT is found in high concentrations in the liver and lower concentrations in the brain, intestines, muscle, adipose tissue, and prostate. Elevated serum levels of ALT tend to be more specific to liver injury than other tissue injury.[i]
AST is found in the liver, muscle, brain, kidneys, pancreas, lungs, and white and red blood cells. Increased release of both enzymes into the bloodstream is a sign of tissue damage which can eventually lead to loss of function.[ii]
In this first part of our 2-part series on the ratios of ALT and AST we will be diving into the ALT:AST ratio and discussing the types of conditions that are associated with an elevated ratio. Part 2 will focus on the AST:ALT ratio!
An increasing ratio of ALT to AST is associated with the closely related disorders of insulin resistance, metabolic syndrome, non-alcoholic fatty liver disease, and cardiovascular disease.[iii] [iv] Research strongly suggests that the ratio may be used as a marker of metabolic health. A health survey of 16,371 adults revealed that increasing ALT:AST ratios correlated with impaired fasting glucose, insulin resistance/HOMA-IR, undiagnosed type 2 diabetes, and declining metabolic health.[v]
Insulin resistance
The presence of insulin resistance should be assessed in view of its role in metabolic syndrome, diabetes, cardiovascular disease, dyslipidemia, and hypertension and extensive research is warranted.
An increased ratio of ALT to AST is independently associated with insulin resistance (IR) and considered a primary marker for the disorder. Researchers in a large cross-sectional study of 8398 adults suggested a cut-off point for ALT:AST of 0.80 in non-centrally obese individuals and 0.78 in the centrally obese for identifying IR.[vi]
Insulin resistance[vii]
In a cross-sectional study of 587 male and 755 female adults, increased risk of insulin resistance was identified by an increasing ratio of ALT to AST in both overweight (BMI greater than 25) and normal weight individuals (BMI less than 25).[ix] The study identified insulin resistance in overweight subjects with an ALT:AST ratio greater than or equal to 1.02. Insulin resistance was identified in normal weight individuals with an ALT:AST ratio of 0.82 or greater, a level associated with a 1.91-fold increase in insulin resistance. The ALT:AST ratio was a better predictor of insulin resistance than blood pressure, low HDL, or ALT and AST alone. The study defined insulin resistance as a HOMA-IR value of 2.5 or greater.
Cardiovascular disease
Cardiovascular disease, insulin resistance, and other metabolic disorders are closely linked, and assessment of the ALT:AST ratio can help confirm this morbid relationship. The ratio of ALT to AST was calculated in 1063 patients with proven coronary artery disease. Research revealed that an ALT:AST ratio of 1.1 was “strongly and significantly” able to predict adverse cardiovascular events in those CAD patients with insulin resistance (defined by a HOMA-R of greater than 2.5).[x]
Metabolic syndrome
The phenomenon of metabolic syndrome is characterized by insulin resistance, glucose intolerance, atherogenic dyslipidemia, hypertension, abdominal obesity, inflammation, and a prothrombotic state and represents a cluster of metabolic abnormalities. Use of the ALT:AST ratio can help identify those at risk for, or in the throes of, metabolic syndrome. A ratio of greater than 1 was observed in 60 adults with established metabolic syndrome.[xi]
The ALT:AST ratio may even help identify those with metabolic syndrome in its “silent” stage. A cross-sectional examination of 1643 male and 1764 female subjects revealed significantly higher ratios of ALT to AST in those identified as having metabolic syndrome. Elevated ALT:AST ratios in both males and females diagnosed with metabolic syndrome significantly correlated with greater waist circumference as well. [xii] The study also confirmed a close association of metabolic syndrome with non-alcoholic fatty liver disease, another metabolic abnormality associated with elevated ALT:AST ratios.
Non-alcoholic liver disease (NAFLD)
The health of the liver is closely tied to blood glucose regulation and insulin resistance, as the liver is responsible for clearing insulin from the bloodstream.[xiii] It comes as no surprise that insulin resistance in turn is closely tied to NAFLD. An increased ALT:AST ratio is considered a surrogate marker for non-alcoholic fatty liver disease, an all-too-common phenomenon associated with accumulation of fat in the liver (hepatosteatosis).[xiv]
The strong association between ALT:AST ratio and NAFLD is evident even in children and adolescents. Those with an ALT:AST ratio of greater than 0.98 had a 2.19-fold greater risk of NAFLD. Low-grade NAFLD was characterized by an ALT:AST ratio of 1.07 while a ratio higher than 1.46 was associated with higher grade NAFLD. Individuals with NAFLD were heavier with a greater waist circumference and had significantly higher blood pressure and dyslipidemia.[xv]
It is imperative to identify NAFLD early as it is closely related to oxidative stress, endothelial dysfunction, adverse cardiovascular events, and metabolic syndrome.[xvi] Evaluation of the ALT:AST ratio can be a significant predictor for hepatosteatosis/NAFLD in individuals with chronic hepatitis C infection as well.[xvii]
An optimal ratio of ALT to AST may reflect metabolic health and absence of liver disease. However, an extremely low ALT:AST may be due to extremely low ALT levels which are in turn associated with frailty and aging.[xviii]
| Condition | ALT:AST ratio |
| Increased risk of insulin resistance (IR) in centrally obese individuals |
Greater than 0.78 |
| Increased risk of IR in NON-centrally obese individuals |
Greater than 0.8 |
| 1.91-fold increased risk of IR in normal weight individuals |
0.82 or greater |
| Increased risk of IR in overweight individuals |
1.02 or greater |
| Increased risk of CVD events in CAD patients with IR |
1.1 |
| Increased risk of metabolic syndrome |
1 or greater |
| 2.19-fold increased risk of NAFLD |
0.98 or greater |
| Increased risk of low-grade NAFLD |
1.07 |
| Increased risk of high-grade NAFLD |
Greater than 1.46 |
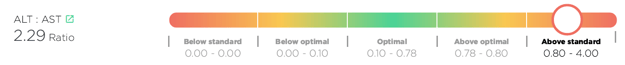
Good news! The ALT:AST ratio is now being automatically calculated by the Optimal DX software if both the ALT and AST are added into the system. No need to do any conversions as the software will do this for you and will now show the result in the Blood Test Results Report:
However, if you simply want to do the calculation manually then please follow these instructions:
The ALT:AST ratio is calculated by dividing the ALT result by the AST result.
Here's an example:
ALT is 22 and the AST is 26: 22 / 26 = 0.85
So, the ALT:AST Ratio in this example is 0.85

[i] Woreta TA, Alqahtani SA. Evaluation of abnormal liver tests. Med Clin North Am. 2014 Jan;98(1):1-16.
[ii] Thapa BR, Walia A. Liver function tests and their interpretation. Indian J Pediatr. 2007 Jul;74(7):663-71. Review. PubMed PMID: 17699976. [R]
[iii] Rief P, Pichler M, Raggam R, et al. The AST/ALT (De-Ritis) ratio: A novel marker for critical limb ischemia in peripheral arterial occlusive disease patients. Medicine (Baltimore). 2016 Jun;95(24):e3843. [R]
[iv] Hall P, Cash J. What is the real function of the liver 'function' tests? Ulster Med J. 2012 Jan;81(1):30-6. [R]
[v] Gowda S, Desai PB, Hull VV, et al. A review on laboratory liver function tests. Pan Afr Med J. 2009 Nov 22;3:17. [R]
[vi] Woreta TA, Alqahtani SA. Evaluation of abnormal liver tests. Med Clin North Am. 2014 Jan;98(1):1-16. [R]
[vii] Giannini E, Risso D, Botta F, et al. Validity and clinical utility of the aspartate aminotransferase-alanine aminotransferase ratio in assessing disease severity and prognosis in patients with hepatitis C virus-related chronic liver disease. Arch Intern Med. 2003 Jan 27;163(2):218-24. [R]
[viii] Newsome PN, Cramb R, Davison SM, et al. Guidelines on the management of abnormal liver blood tests. Gut. 2018 Jan;67(1):6-19. [R]
[ix] Hall P, Cash J. What is the real function of the liver 'function' tests? Ulster Med J. 2012 Jan;81(1):30-6. [R]
[x] Giannini E, Risso D, Botta F, et al. Validity and clinical utility of the aspartate aminotransferase-alanine aminotransferase ratio in assessing disease severity and prognosis in patients with hepatitis C virus-related chronic liver disease. Arch Intern Med. 2003 Jan 27;163(2):218-24. [R]
[xi] Botros M, Sikaris KA. The de ritis ratio: the test of time. Clin Biochem Rev. 2013 Nov;34(3):117-30. Review. [R]
[xii] Botros M, Sikaris KA. The de ritis ratio: the test of time. Clin Biochem Rev. 2013 Nov;34(3):117-30. Review. [R]
[xiii] Kawachi I, Robinson GM, Stace NH. A combination of raised serum AST:ALT ratio and erythrocyte mean cell volume level detects excessive alcohol consumption. N Z Med J. 1990 Apr 11;103(887):145-8. [R]
[xiv] Lala V, Goyal A, Bansal P, Minter DA. Liver Function Tests. 2020 Mar 27. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.Available from [R]
[xv] Thapa BR, Walia A. Liver function tests and their interpretation. Indian J Pediatr. 2007 Jul;74(7):663-71. Review. [R]
[xvi] Alempijevic T, Krstic M, Jesic R, et al. Biochemical markers for non-invasive assessment of disease stage in patients with primary biliary cirrhosis. World J Gastroenterol. 2009 Feb 7;15(5):591-4. [R]
[xvii] Hall P, Cash J. What is the real function of the liver 'function' tests? Ulster Med J. 2012 Jan;81(1):30-6. [R]
[xviii] Rief P, Pichler M, Raggam R, et al. The AST/ALT (De-Ritis) ratio: A novel marker for critical limb ischemia in peripheral arterial occlusive disease patients. Medicine (Baltimore). 2016 Jun;95(24):e3843. doi: 10.1097/MD.0000000000003843. Erratum in: Medicine (Baltimore). 2016 Aug 07;95(31):e5074. [R]
[xix] Rej R. Aminotransferases in disease. Clin Lab Med. 1989 Dec;9(4):667-87. PMID: 2686908. [R]
[xx] Lin S, Tang L, Jiang R, et al. The Relationship Between Aspartate Aminotransferase To Alanine Aminotransferase Ratio And Metabolic Syndrome In Adolescents In Northeast China. Diabetes Metab Syndr Obes. 2019 Nov 18;12:2387-2394[R]
[xxi] Hanley AJ, Williams K, Festa A, et al. Liver markers and development of the metabolic syndrome: the insulin resistance atherosclerosis study. Diabetes. 2005 Nov;54(11):3140-7. [R]