Candida albicans is the most common yeast found in the body, including in the gastrointestinal tract. It can be harmless at low levels but pathogenic when it overgrows and changes from unicellular yeast to a filamentous hyphal form.
It can become a systemic threat if it moves from the GI tract into the bloodstream. This translocation is more likely with a compromised intestinal barrier, immune dysfunction, and imbalances in gut microbiota composition.
Unhealthy diet and lifestyle patterns contribute to inflammatory pathogenesis and gut dysbiosis
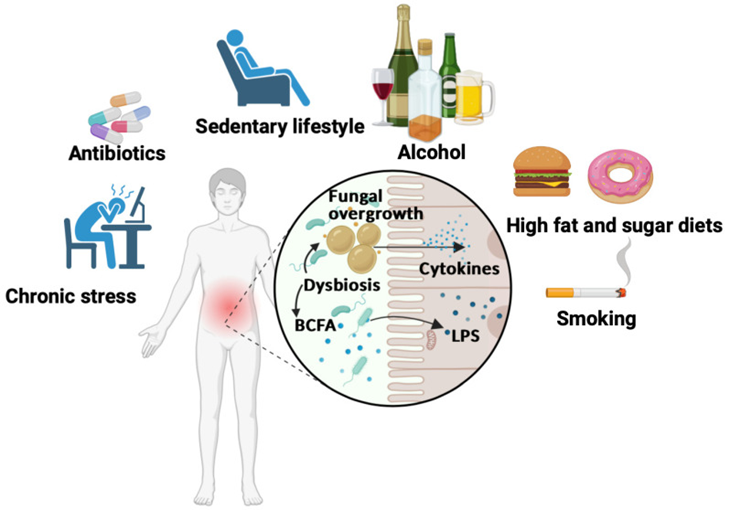
Diets high in fat and sugar, smoking, excessive alcohol consumption, lack of physical activity, prolonged use of antibiotics, and chronic psychological stress all contribute to the development of gut dysbiosis. These diets cause an increase in branched-chain fatty acid (BCFA) production and populations of photobiont bacteria, such as E. coli, which produce lipopolysaccharides (LPS), as well as alteration of the intestinal barrier. Significant overgrowth of fungi is also observed, in particular C. albicans, in the gut during dysbiosis. All these factors induce the production of pro-inflammatory cytokines and leakage of pathogen-derived compounds, including LPS and fungal cell wall fractions, into the blood.
A balanced, low-sugar, plant-based, whole-food diet, such as the Mediterranean diet, can help support GI microbiota diversity and help keep C. albicans under control.
Probiotic therapy can help restore microbial diversity and help disrupt C. albicans biofilms. Potentially beneficial probiotics include Bifidobacterium and Lactobacilli species, and Saccharomyces boulardii. Prebiotics, including fructo-oligosaccharides as tolerated, can provide food and fuel to the beneficial GI microbes and contribute to a healthy microbiota composition.
The beneficial effects of a diet high in vegetable fiber, vitamins, micronutrients, omega-3 polyunsaturated fatty acids, and probiotics/prebiotics on the gut microbiota.
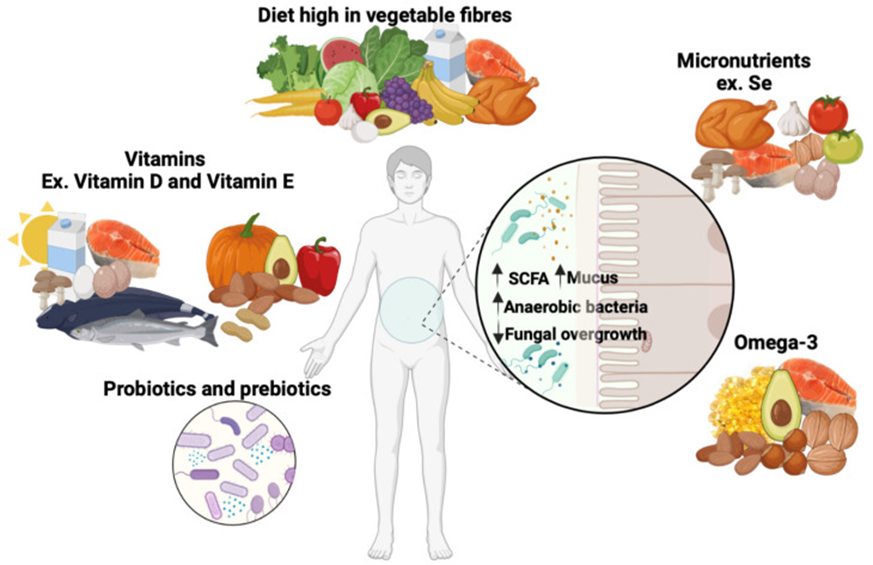
A diet based on whole plant foods, including vegetables, fruits, whole grains, nuts, and seeds, associated with a portion of animal products (meat, dairy, and eggs) or seafood provides significant amounts of fiber, antioxidants, as well as vitamins like vitamins D and E, omega-3 fatty acids, and micronutrients such as selenium. In addition, a probiotic or prebiotic supplement is important to prevent gut dysbiosis. This diet contributes to an increase in short-chain fatty acid (SCFA) production and mucus secretion, as well as an increase in anaerobic bacteria such as Lactobacillus and Bifidobacterium species. Pathogenic fungi are significantly reduced in subjects consuming this diet. These conditions all promote gut microbiota biodiversity.
Plants produce thousands of natural compounds that protect not only the plant but humans as well. Several of these compounds can help combat fungal infections and can be found in:
Antifungal properties of natural compounds obtained from a variety of foods and plants known in traditional medicine
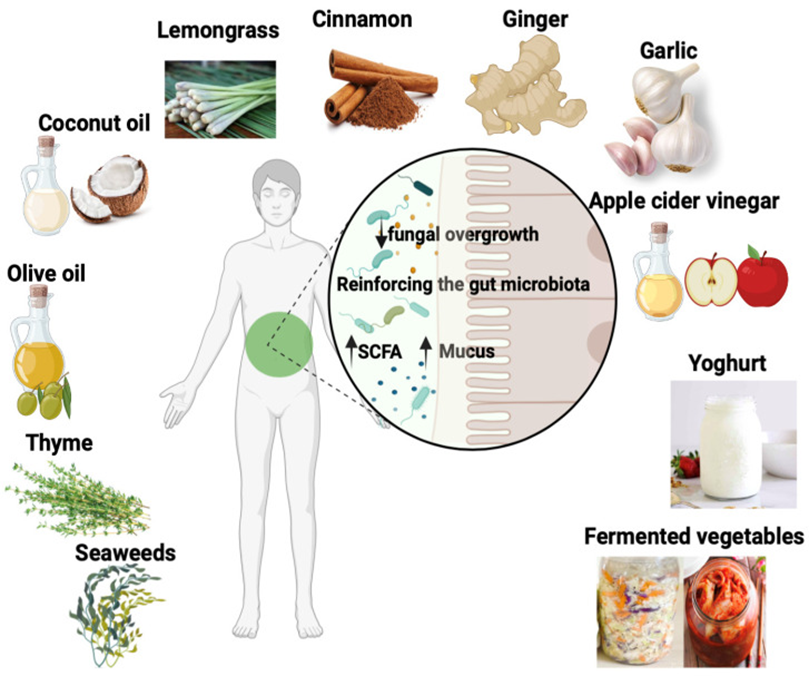
These foods and plants include garlic (Allium sativum), cinnamon (Cinnamomum verum), lemongrass (Cymbopogon citratus), coconut oil, ginger, seaweed (algae), thyme, olive oil, fermented vegetables, apple cider vinegar, and yogurt. These plants and foods reinforce the biodiversity of the gut microbiota, contributing to an increase in SCFA production and mucus secretion. In addition, pathogenic fungi are significantly reduced by these plants.
Adopting a healthy plant-based diet along with healthy protein sources, including fish and seafood, can help balance the gastrointestinal microbiome, maintain healthy intestinal permeability, and reduce the risk of Candida infection.
Supplement as needed with micronutrients, omega-3 fatty acids, and natural compounds from plant foods, including garlic, ginger, apple cider vinegar, cinnamon, coconut oil, olive oil, seaweed, thyme, and lemongrass.
Adopting healthy lifestyle habits is also essential and should include physical activity, stress management, moderation in alcohol consumption, and not smoking, ever.
Jawhara S. Healthy Diet and Lifestyle Improve the Gut Microbiota and Help Combat Fungal Infection. Microorganisms. 2023 Jun 11;11(6):1556. doi: 10.3390/microorganisms11061556. PMID: 37375058; PMCID: PMC10302699 This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).