Taurine is a conditionally essential sulfur-containing amino acid vital to human health
Taurine is one of the few amino acids not incorporated into proteins despite it being one of the most abundant amino acids found in organs throughout the body. Taurine insufficiency is associated with cardiomyopathy, kidney dysfunction, pancreatic beta cell dysfunction, and severe eye damage (Ripps 2012).
Taurine is currently considered conditionally essential as the body can produce it but not sufficiently during stress or pathological conditions. Therefore, exogenous sources of taurine are “conditionally” required. Vitamin B6 is necessary for endogenous taurine synthesis (Lourenco 2002).
Dietary sources of taurine include seafood, meat, and milk. However, it can also be produced in the liver (primarily) from cysteine or methionine. Taurine is abundant in “excitatory tissues,” including the brain, heart, skeletal muscle, and retina (Jong 2021), as well as the liver, platelets, and white blood cells. It can also be produced to some extent in the kidney and brain (Baliou 2021).
Taurine helps sustain electron transport chain activity, maintain glutathione stores, upregulate antioxidant activity, improve cell membrane stability, counteract inflammation, prevent excess cellular calcium accumulation (Baliou 2021), facilitate bile acid conjugation, and regulate blood glucose levels (Sak 2019).
Research indicates that taurine may be protective against mitochondrial dysfunction and associated disorders, including metabolic syndrome, cardiovascular disease, neurological disorders, and cancer. Such pathologies are characterized by increased oxidative stress, cell damage, decreased energy generation, and impaired mitochondrial production (Jong 2021).
Taurine supports mitochondrial health
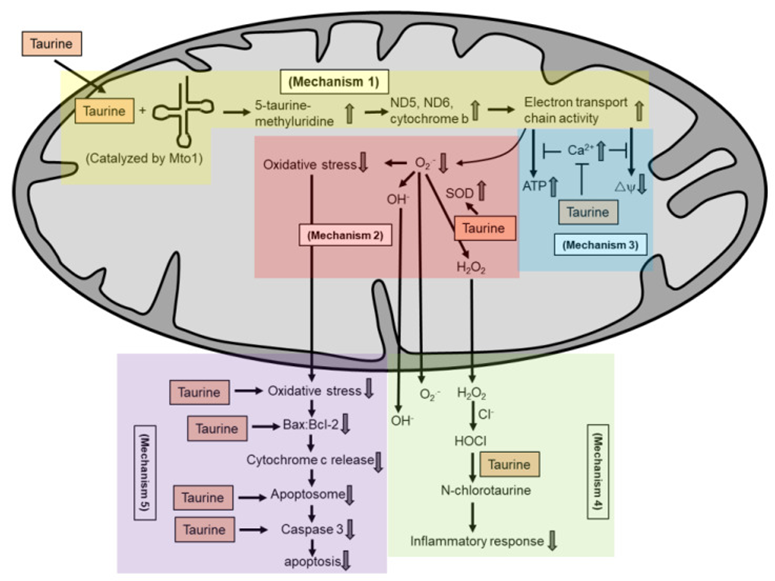
Taurine is not known as a radical scavenger. Several potential mechanisms by which taurine exerts its antioxidant activity in maintaining mitochondria health include: taurine conjugates with uridine on mitochondrial tRNA to form a 5-taurinomethyluridine for proper synthesis of mitochondrial proteins (mechanism 1), which regulates the stability and functionality of respiratory chain complexes; taurine reduces superoxide generation by enhancing the activity of intracellular antioxidants (mechanism 2); taurine prevents calcium overload and prevents reduction in energy production and the collapse of mitochondrial membrane potential (mechanism 3); taurine directly scavenges HOCl to form N-chlorotaurine in inhibiting a pro-inflammatory response (mechanism 4); and taurine inhibits mitochondria-mediated apoptosis by preventing caspase activation or by restoring the Bax/Bcl-2 ratio and preventing Bax translocation to the mitochondria to promote apoptosis (mechanism 5).
Source: Jong, Chian Ju et al. “The Role of Taurine in Mitochondria Health: More Than Just an Antioxidant.” Molecules (Basel, Switzerland) vol. 26,16 4913. 13 Aug. 2021, doi:10.3390/molecules26164913 This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Taurine insufficiency in chronic disease
Taurine is essential to cardiac function. It accounts for more than 50% of the free amino acids in cardiac tissue and appears to support heart health in several ways, including (Baliou 2021):
- Ameliorating endothelial damage and dysfunction
- Protecting against homocysteine-induced damage
- Reducing potential damage by oxidized LDL
- Decreasing production of apolipoprotein B100
- Modulating HMG-CoA reductase and excess cholesterol synthesis
- Working synergistically with omega-3 fatty acids and magnesium
- Protecting cardiac tissue from toxins and calcium overload
- Preventing or reducing atherosclerosis
- Protecting against ischemia-reperfusion
Taurine plays a role in glucose homeostasis and insulin secretion as well, and taurine insufficiency is associated with diabetes and its complications, including diabetic neuropathy (Sak 2019).
Taurine may reduce the oxidative stress, inflammation, and glycation associated with diabetes. A randomized double-blind, placebo-controlled trial comprising 50 type 2 diabetes patients found that those supplemented with 1000 mg of taurine three times daily for 8 weeks had significant increases in superoxide dismutase (SOD) and catalase (CAT) and significantly reduced hs-CRP, malondialdehyde (MDA), and TNF-alpha following supplementation. The placebo group experienced decreases in SOD, CAT, and total antioxidant capacity and increases in MDA, hs-CRP, TNF-a, and IL-6 cytokines (Maleki 2020).
The role of taurine in neuromodulation has been studied as well. Taurine can decrease glutamate toxicity during a stroke, which reduces associated oxidative stress and calcium overload. Taurine is released from CNS cells and is protective following stroke and other pathological conditions. It can mimic some of the actions of GABA and balance inhibition and excitation of CNS neurons. However, while acute taurine administration activates the GABA receptor, chronic administration can downregulate it (Schaffer 2018).
Taurine-mediated protection against pathology and disease
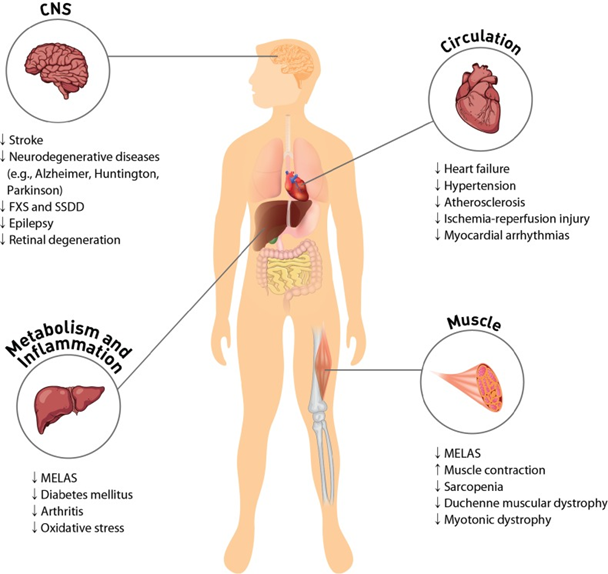
High concentrations of taurine in most cells regulate physiological function of excitable tissues and mitochondria. Taurine protects CNS by decreasing ER stress and antagonizing neurotransmitter receptors of GABAA, glycine and NMDA. Protection of the cardiovascular system by taurine occurs through regulation of cell signaling, such as Ca2+ transport, ROS generation and protein phosphorylation. Supplementation of taurine ameliorates symptoms of MELAS and diabetes mellitus. The anti-inflammatory activity of taurine involves either the formation of taurochloramine in neutrophils or the attenuation of nitric oxide and prostaglandin E2 in inflammatory diseases, such as rheumatoid arthritis and osteoarthritis. Taurine depletion or taurine transporter KO leads to cardiac and skeletal muscle dysfunction. Taurine prevents sarcopenia in aged person by minimizing gradual muscle loss. CNS: central nervous system; FXS: fragile X syndrome; SSDD: succinic semialdehyde dehydrogenase deficiency; MELAS: mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes.
Source Schaffer, Stephen, and Ha Won Kim. “Effects and Mechanisms of Taurine as a Therapeutic Agent.” Biomolecules & therapeutics vol. 26,3 (2018): 225-241. doi:10.4062/biomolther.2017.251. This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/)
Taurine Supplementation
Taurine supplementation is an approved medical therapy for congestive heart failure and mitochondrial myopathy in Japan. It may help alleviate the metabolic dysfunction and oxidative stress associated with pathologies such as cardiovascular disease, metabolic syndrome, cancer, and neurological disorders in adults. In infants, inadequate taurine supplementation can lead to impaired bile acid secretion, compromised lipid absorption, hepatic dysfunction, and retinal disorders due to the infant’s decreased ability to produce it de novo (Jong 2021).
In general, supplementation may be indicated for those at risk of deficiency, including individuals with chronic liver, kidney, or heart failure or those reliant on parenteral nutrition (Lourenco 2002).
Plasma levels of taurine vary with consumption and specimen. While average fasting plasma taurine is ~44 umol/L, whole blood taurine concentrations are higher at ~227 umol/L. One pharmacokinetic study found that 4 grams of taurine increased plasma levels from a baseline fasting level of 30-60 umol/L to 500 umol/L in 1.5 hours and back to baseline in 6.5 hours (Jong 2021).
Lower doses of 3 mg/kg were found to improve heart function in congestive heart failure patients, while higher doses may be used to enhance athletic performance (Baliou 2021).
A qualified health professional should supervise taurine supplementation, which may include 500-1000 mg of taurine twice daily in adults (Noland 2020).
ODX Optimal Takeaways
Taurine is a conditionally essential amino acid. Consumption via food or supplements may be indicated in times of increased oxidative stress or metabolic dysfunction, including heart disease, diabetes, cancer, and neurological disorders.
Taurine benefits include:
- Support of mitochondrial function
- Facilitation of antioxidant activity
- Reduction of oxidative stress and inflammation
- Improvement of blood glucose regulation
- Promotion of neurotransmitter balance
- Protection of cardiac tissue and function
Taurine supplementation may be indicated in the following:
- Diabetes
- Cardiomyopathy
- Oxidative stress
- Stroke
- Infancy
- Reliance on parenteral nutrition
- Vitamin B6 insufficiency
- Vegans
References
Baliou, Stella et al. “Protective role of taurine against oxidative stress (Review).” Molecular medicine reports vol. 24,2 (2021): 605. doi:10.3892/mmr.2021.12242
Jong, Chian Ju et al. “The Role of Taurine in Mitochondria Health: More Than Just an Antioxidant.” Molecules (Basel, Switzerland) vol. 26,16 4913. 13 Aug. 2021, doi:10.3390/molecules26164913
Lourenco, R, and M E Camilo. “Taurine: a conditionally essential amino acid in humans? An overview in health and disease.” Nutricion hospitalaria vol. 17,6 (2002): 262-70.
Maleki, Vahid et al. “The effects of taurine supplementation on oxidative stress indices and inflammation biomarkers in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled trial.” Diabetology & metabolic syndrome vol. 12 9. 29 Jan. 2020, doi:10.1186/s13098-020-0518-7
Noland, Diana, Jeanne A. Drisko, and Leigh Wagner, eds. Integrative and functional medical nutrition therapy: principles and practices. Springer Nature, 2020.
Ripps, Harris, and Wen Shen. “Review: taurine: a "very essential" amino acid.” Molecular vision vol. 18 (2012): 2673-86.
Sak, Duygu et al. “The Relationship between Plasma Taurine Levels and Diabetic Complications in Patients with Type 2 Diabetes Mellitus.” Biomolecules vol. 9,3 96. 11 Mar. 2019, doi:10.3390/biom9030096
Schaffer, Stephen, and Ha Won Kim. “Effects and Mechanisms of Taurine as a Therapeutic Agent.” Biomolecules & therapeutics vol. 26,3 (2018): 225-241. doi:10.4062/biomolther.2017.251







