Atherosclerosis is an oxidative inflammatory process characterized by the progressive buildup of plaque within medium and large arteries. Plaque accumulation impedes blood flow, reduces oxygen delivery, and can eventually block the artery completely, leading to myocardial infarction or stroke. Atherosclerosis is the primary cause of ischemic heart disease, stroke, and sudden death.
Development of atherosclerotic lesions
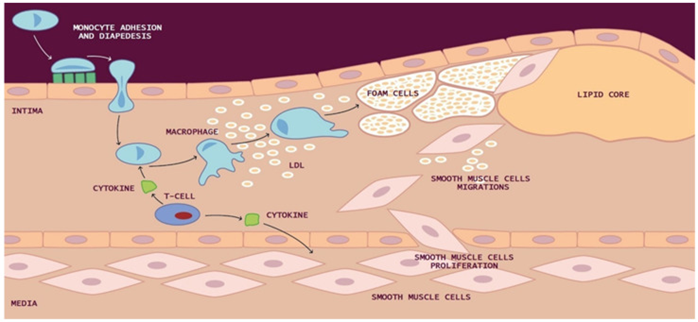
In the intima, reactive oxygen species (ROS) cause the oxidation of low-density lipoprotein (LDL) and promote macrophage internalization of oxidized LDL (ox-LDL).
Macrophages can also uptake LDL by micropinocytosis or in its aggregated form as cholesterol complexes by phagocytosis to form lipid-laden macrophages called “foam cells.”
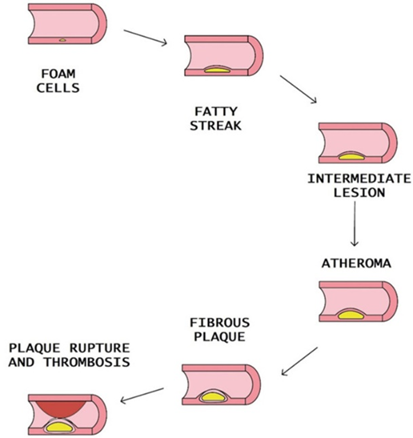
Yellow foam cells aggregate on the arterial walls and cause the development of fatty streaks. Smooth muscle cells (SMCs) migrate from the media to the intima and multiply, forming a fibrous atherosclerotic plaque cap from the fatty streak.
Inflammation, endothelial dysfunction, disruption of vascular homeostasis, and modification/oxidation of low-density lipoprotein (oxLDL) appear to be the first steps in the development of atherosclerosis. Additional risk factors include hypertension, diabetes, cigarette smoking, genetic factors, infectious organisms, excess free radicals, and elevated homocysteine.
Certain serum biomarkers and biomarker patterns are associated with the progression of atherosclerosis and its association with adverse events.
|
Biomarkers |
Function in Atherosclerosis |
|
Ox-LDL |
Initiation and progression of atherosclerosis by inducing dysfunction in endothelial cells (ECs) An excess of oxygen and nitrogen free radicals modify lipids, proteins, and carbohydrates within the intima, the innermost lining of the artery, altering their behavior and function. Oxidized LDL, in particular, plays a nefarious role in promoting atherosclerosis. It induces endothelial dysfunction, triggers an inflammatory immune response, and activates macrophages. These macrophages then take up oxidized LDL, become foam cells, and create the fatty streaks that characterize atherosclerotic plaque. This plaque can become unstable and rupture, triggering coagulation, forming blood clots and thrombi, and eventually blocking the artery. High-density lipoprotein may protect against CVD by removing lipids from the endothelium and impeding the production of foam cells. |
|
sdLDLs |
Provide oxidized cholesterol for developing atherosclerotic plaque Have an extended circulation time, are prone to oxidation, and easily penetrate the intima. Significantly increase atherosclerosis risk, and their elevation is considered a risk factor for cardiovascular disease. Associated with phenotype B, metabolic disorders, including obesity and type 2 diabetes, coronary heart disease, and hypertriglyceridemia. |
|
Lp(a) |
Pro-inflammatory action on the arterial wall due to oxidized phospholipids and atherogenic and pro-thrombotic activity associated with the homology with plasminogen Consists of a lipoprotein molecule bound to apolipoprotein B, the protein portion of LDL. Is proinflammatory, prothrombotic, and carries atherogenic oxidized phospholipids. |
|
CRP |
Non-specific indicator of inflammation upregulated due to vascular disease. Independently predicts primary and secondary coronary heart disease events Upregulates cell adhesion molecules, enhances release of MCP-1, facilitates the uptake of LDL into macrophages Triggered by various mediators, including interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor (TNF). Binds the cell membrane of activated monocytes but not resting monocytes. Induces the polarization of monocytes towards the M1 phenotype and converts M2 monocytes into the M1 phenotype, thereby promoting the recruitment of monocytes into the plaque. Is found within atherosclerotic plaque and damaged vessel walls, where it plays a role in its secretion Can be produced outside the liver, including by cell types within atherosclerotic plaque which may result in concentrations several times higher within atherosclerotic plaques compared with serum levels. CRP receptors have been identified in various other cell types, such as neutrophils, resident macrophages, and endothelial cells. High-sensitivity CRP testing can detect low levels of CRP that may be associated with chronic low-level inflammation. |
|
M1-like macrophages |
Induce the recruitment and activation of other macrophages, T cells, B cells, and dendritic cells, promoting inflammation and advancing atherosclerotic plaque development. The accumulation of intravascular lipids recruits monocytes to atherosclerosis-prone areas, where they differentiate into macrophages. Subsequently, these macrophages undergo metabolic reprogramming in response to atherogenic stimuli present in the plaque microenvironment, such as modified lipoproteins and hypoxia. |
|
M2-like macrophages |
Secrete anti-inflammatory and pro-fibrotic mediators and help limit inflammation, thus inhibiting the progression of atherosclerosis. M2-like macrophages secrete anti-inflammatory and pro-fibrotic mediators and help limit inflammation, thus inhibiting the progression of atherosclerosis. Early regression of atherosclerosis can occur through increased apoptosis of cholesterol-laden macrophages, followed by the uptake of these apoptotic cells by neighboring macrophages. |
Steps of atheromatous plaque formation, progression, and rupture

Della Corte, Vittoriano et al. “Atherosclerosis and Its Related Laboratory Biomarkers.” International journal of molecular sciences vol. 24,21 15546. 24 Oct. 2023, doi:10.3390/ijms242115546 This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).