Overview of endocannabinoids and the ECS
Humans produce endocannabinoids such as 2-arachidonoylglycerol (2-AG) and arachidonylethanolamide (anandamide/AEA), derivatives of the omega-6 fatty acid arachidonic acid. Endocannabinoids work with designated receptors in the brain and body as part of the endocannabinoid system (ECS). Endocannabinoids are involved in several physiological processes (Smiarowska 2022):
Cannabinoids help regulate:
- Appetite and digestive function
- Bone development and density
- Cardiovascular function
- Emotional state and mood
- Homeostasis
- Immune function
- Inflammation
- Learning and memory
- Metabolism, energy expenditure
- Pain inhibition
- Psychomotor activity
- Reproduction
- Sleep/wake cycles
- Stress management
Dysregulation of the ECS can contribute to
- Increased inflammation
- Neurodegenerative processes
- Pain
- Psychiatric disturbance
Phytocannabinoids
Therapeutic use of the cannabis plant dates to at least 2,727 BC in China. It was integrated into Western medicine in the early 1800s by surgeon W.B. O’Shaughnessy, who prescribed it as a sedative, anti-inflammatory, anti-spasmodic, and anti-convulsant.
The cannabis (hemp) plant produces phytocannabinoids, while the human body produces endocannabinoids. They both appear to interact with the human endocannabinoid system. Phytocannabinoids include (Daniela 2020):
- Delta 9-tetrahydrocannabinol Δ9-THC
- Delta 8-tetrahydrocannabinol Δ8-THC
- Cannabidiol (CBD)
- Cannabigerol (CBG)
- Cannabinol (CBN)
- Cannabinodiol (CBND)
- Cannabitriol (CBT)
- Cannabielsoin (CBE)
- Cannabicyclol (CBL)
- Cannabichromene (CBC)
The ratio between the primary cannabinoids THC and CBD determines the classification of a particular plant
- THC/CBD of greater than 1 designates it as a “drug type”
- THC/CBD of 1 designates it as an “intermediate type”
- THC/CBD of less than 1 designates it as a “fiber type"
Tetrahydrocannabinol produces a psychoactive effect in the brain and is used medicinally to stimulate appetite, prevent nausea and vomiting, reduce muscle spasticity, address bladder dysfunction, and treat Tourette syndrome. Delta 9- and Delta 8-THC may be used recreationally for their psychoactive effects. However, this effect can lead to cognitive disturbance, short-term memory loss, decreased reaction time, loss of coordination, attention deficit, and severe panic. Delta 8-THC is approximately 30% less psychotropic, may be neuroprotective, and may have the potential to reduce the size of malignant tumors.
CBD does not exert a psychoactive effect and is currently considered the most therapeutic phytocannabinoid with beneficial effects in epilepsy, neurological disorders, anxiety, depression, chronic pain, and even cancer. CBD is currently being researched for Parkinson’s, Huntington’s, Alzheimer’s, multiple sclerosis, ALS, and cerebral ischemia/hypoxia. CBD can also counteract the psychoactive effects of THC. However, CBD may interact with pharmaceutical drugs, so dosing should be regulated (Daniela 2020).
National Academies of Sciences research review
The National Academies of Sciences’ list of health topics and prioritized endpoints with regard to the health effects of cannabis and cannabinoids includes:
- Therapeutic effects
- Chronic pain; cancer, chemotherapy-induced nausea/vomiting; anorexia and weight loss; irritable bowel syndrome; epilepsy; spasticity related to multiple sclerosis or spinal cord injury; Tourette syndrome; amyotrophic lateral sclerosis; Huntington’s disease; Parkinson’s disease; dystonia; dementia; glaucoma; traumatic brain injury; addiction; anxiety; depression; sleep disorders; posttraumatic stress disorder; schizophrenia and other psychoses
- Cancer
- Lung cancer; head and neck cancer; testicular cancer; esophageal cancer; other cancer
- Cardiometabolic risk
- Acute myocardial infarction; stroke; metabolic dysregulation, metabolic syndrome, prediabetes, and diabetes mellitus
- Respiratory disease
- Pulmonary function; chronic obstructive pulmonary disorder; respiratory symptoms (including chronic bronchitis); asthma
- Immunity
- Immune function; infectious disease
Report Conclusions
There is conclusive or substantial evidence that cannabis or cannabinoids are effective:
- For the treatment of chronic pain in adults (cannabis)
- As antiemetics in the treatment of chemotherapy-induced nausea and vomiting (oral cannabinoids)
- For improving patient-reported multiple sclerosis spasticity symptoms (oral cannabinoids)
There is moderate evidence that cannabis or cannabinoids are effective for:
- Improving short-term sleep outcomes in individuals with sleep disturbance associated with obstructive sleep apnea syndrome, fibromyalgia, chronic pain, and multiple sclerosis (cannabinoids, primarily nabiximols)
There is limited evidence that cannabis or cannabinoids are effective for:
- Increasing appetite and decreasing weight loss associated with HIV/AIDS (cannabis and oral cannabinoids)
- Improving clinician-measured multiple sclerosis spasticity symptoms (oral cannabinoids)
- Improving symptoms of Tourette syndrome (THC capsules)
- Improving anxiety symptoms, as assessed by a public speaking test, in individuals with social anxiety disorders (cannabidiol)
- Improving symptoms of posttraumatic stress disorder (nabilone; a single, small, fair-quality trial)
Clinical endocannabinoid deficiency
Physiological and genetic alterations in the ECS theoretically lead to increased pain and digestion, mood, and sleep disruptions. The most significant evidence for clinical endocannabinoid deficiency (CED) is present in migraine, fibromyalgia, and irritable bowel syndrome (IBS). A strong case can be advanced for unifying pathophysiological trends in the three conditions (Russo 2016):
- All manifest hyperalgesic states must be clinically diagnosed based on subjective criteria, as all lack characteristic tissue pathology or easily accessible objective laboratory findings
- All are diagnoses of exclusion that often generate extensive negative diagnostic work-ups
- They display elevated incidence of anxiety and depression (in a chicken vs. egg dilemma) and have been labeled psychosomatic in origin or worse, wastebasket diagnoses, at one time or another by skeptical clinicians
- Comorbidity is quite clear in the three diagnoses.
- Primary headaches co-occurred in 97% of 201 fibromyalgia patients
- 6% of 101 chronic daily headache (transformed migraine) subjects also fit the clinical criteria of fibromyalgia
- 6% of IBS subjects were also diagnosable with fibromyalgia
- 32% of fibromyalgia patients also fit the clinical criteria for IBS
- While some patients suffer from only one of these syndromes, the lifetime risk of developing another or all three is quite common
- Additional disorders that may be associated with a disruption in the ECS include:
- Neonatal failure to thrive
- Cystic fibrosis
- Causalgia
- Brachial plexopathy
- Phantom limb pain
- Infantile colic
- Glaucoma
- Dysmenorrhea
- Hyperemesis gravidarum
- Repetitive miscarriages
- Post-traumatic stress disorder (PTSD)
- Bipolar disease
Comorbidity of migraine, fibromyalgia, and irritable bowel syndrome
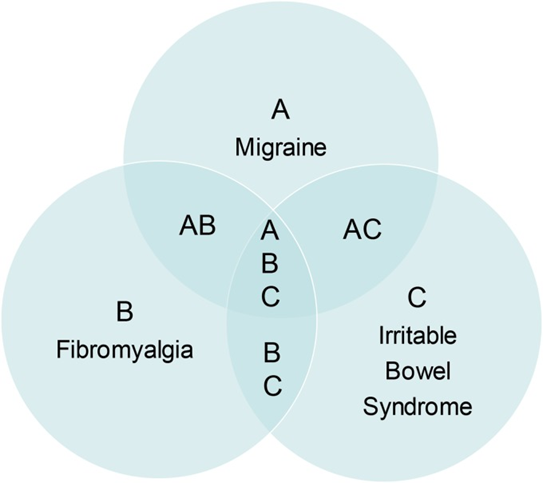
Source: Russo, Ethan B. “Clinical Endocannabinoid Deficiency Reconsidered: Current Research Supports the Theory in Migraine, Fibromyalgia, Irritable Bowel, and Other Treatment-Resistant Syndromes.” Cannabis and cannabinoid research vol. 1,1 154-165. 1 Jul. 2016, doi:10.1089/can.2016.0009. This Open Access article is distributed under the terms of the Creative Commons License (http://creativecommons.org/licenses/by/4.0)
CBD research review
According to a systematic literature review of studies evaluating the efficacy of 4-6 week use of CBD (Larsen 2020):
- 20 randomized controlled studies found that CBD had:
- A positive effect on anxiety, schizophrenia, and tobacco addiction
- A minor or no effect on inflammatory bowel disease (IBDs Crohn’s and ulcerative colitis), dyslipidemia, and cannabis use disorder
- Three observational studies found that CBD had a positive effect compared to baseline.
- In general:
- The most common side effects of CBD were fatigue, diarrhea, and appetite or weight change.
- CBD had a positive effect on acutely psychotic patients but not on chronic schizophrenics treated with antipsychotic drugs.
- Use of CBD for epilepsy or psychotic disorders had fewer side effects compared to other available treatments.
- Most studies found that oral CBD reduced anxiety.
- Most studies used purified CBD, which can have a “bell-shaped” response.
- However, CBD-rich extracts that contain other cannabinoids may be even more effective due to the “entourage effect.” Individual dosing efficacy can vary.
Neurological effects
Cannabidiol’s effects on the nervous system include regulation of neurotransmitter release, oxidative stress reduction, inflammation modulation, and management of neuronal excitability. It is currently considered a promising treatment for a variety of neurological disorders, including epilepsy, neuropathic pain, multiple sclerosis, Parkinson’s, and Alzheimer’s (Singh 2023).
Meta-analysis of observational studies evaluating CBD in epilepsy suggests that mixed extracts exerting a synergistic entourage effect may be better tolerated and have efficacy at a lower dose than purified CBD, e.g., 6.0 mg/kg/day versus 25.3 mg/kg/day, primarily in children and adolescents (Pamplona 2018).
Gastrointestinal effects
The endocannabinoid system regulates gastrointestinal propulsion, secretions, inflammation, and nociception. Cannabis was used effectively in the 1900s to treat the secretory diarrhea associated with cholera, a treatment validated by modern technology (Russo 2016).
The positive effects of CBD on the GI tract, mood, and anxiety make it a promising therapy for irritable bowel syndrome, which is characterized by abdominal pain, spasms, visceral hypersensitivity, and altered bowel movements (Brugnatelli 2020).
A prospective, double-blind, randomized 8-week placebo-controlled trial of a CBD-rich oral supplement was conducted in 56 patients with mild-to-moderate Crohn’s disease. Results demonstrated significant improvement in quality of life and clinical presentation despite no significant improvements in serum CRP or stool calprotectin. The test supplement comprised 160 mg of CBD and 40 mg of THC per mL, i.e., 165 CBD and 4% THC in a ratio of 4:1 CBD:THC. Therapy was initiated at 16 mg CBD and 4 mg THC per day, titrated up according to symptom relief to a maximum of 320 mg CBD, 80 mg THC daily (Naftali 2021).
Adverse effects of THC-rich cannabis
Short-term adverse effects of cannabis appear to be primarily associated with THC and can include (Smiarowska 2022):
- Cannabis use disorder and addiction
- Confusion
- Disorientation
- Dizziness
- Drowsiness
- Dry mouth
- Euphoria
- Exacerbation of psychoses
- Fatigue
- Hallucinations
- Impairment of hand-eye coordination, attention, vigilance, and time and distance perception
- Loss of balance
- Nausea
- Short-term memory loss
- Somnolence
- Vomiting
Acute use of higher dose THC-containing cannabis (i.e., marijuana) may increase the risk of cardiovascular complications, including atrial fibrillation, elevated heart rate, and orthostatic hypotension. However, chronic use is associated with increased blood volume, decreased heart rate, and reduced circulatory response to exercise, suggestive of increased parasympathetic activity and decreased sympathetic activity. Cannabis use has also been associated with the modulation of cardiovascular disease risk factors, protection from cardiac tissue ischemia, reduced tobacco use, smaller waist size, lower fasting insulin and HOMA-IR values, and reduced prevalence of diabetes mellitus (Goyal 2017).
In a retrospective analysis of hospitalized myocardial infarction patients, those reporting marijuana use were significantly less likely to die, experience shock, or require invasive treatment with an intra-aortic balloon pump. They were more likely to require mechanical ventilation (Johnson-Sasso 2018).
ODX Optimal Takeaways
- Cannabinoids are produced in the body and also found in nature in the cannabis plant.
- Cannabinoids interact with the endocannabinoid receptors in the body and can influence several physiological systems, including the central nervous and musculoskeletal systems.
- CBD appears to be the more therapeutic phytocannabinoid with fewer side effects than psychoactive THC.
- CBD can counteract the psychoactive effects of THC.
- Optimal dosing of cannabis compounds has not been established, and individual tolerance and clinical indications should be considered.
References
Brugnatelli, Viola et al. “Irritable Bowel Syndrome: Manipulating the Endocannabinoid System as First-Line Treatment.” Frontiers in neuroscience vol. 14 371. 21 Apr. 2020, doi:10.3389/fnins.2020.00371
Daniela, ONA Andreea, Sorin MUNTEAN, and Leon MUNTEAN. "The phytocannabinoides from Cannabis sativa L. An overview." Hop Med Plants 27 (2020): 109-16.
Goyal, Hemant et al. “Role of cannabis in cardiovascular disorders.” Journal of thoracic disease vol. 9,7 (2017): 2079-2092. doi:10.21037/jtd.2017.06.104
Johnson-Sasso, Cecelia P et al. “Marijuana use and short-term outcomes in patients hospitalized for acute myocardial infarction.” PloS one vol. 13,7 e0199705. 11 Jul. 2018, doi:10.1371/journal.pone.0199705
Larsen C, Shahinas J. Dosage, Efficacy and Safety of Cannabidiol Administration in Adults: A Systematic Review of Human Trials. J Clin Med Res. 2020;12(3):129-141. doi:10.14740/jocmr4090. This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License,
Naftali, Timna et al. “Oral CBD-rich Cannabis Induces Clinical but Not Endoscopic Response in Patients with Crohn's Disease, a Randomised Controlled Trial.” Journal of Crohn's & colitis vol. 15,11 (2021): 1799-1806. doi:10.1093/ecco-jcc/jjab069
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington (DC): National Academies Press (US); 2017 Jan 12. 4, Therapeutic Effects of Cannabis and Cannabinoids. Available from: https://www.ncbi.nlm.nih.gov/sites/books/NBK425767/
Pamplona, Fabricio A et al. “Potential Clinical Benefits of CBD-Rich Cannabis Extracts Over Purified CBD in Treatment-Resistant Epilepsy: Observational Data Meta-analysis.” Frontiers in neurology vol. 9 759. 12 Sep. 2018, doi:10.3389/fneur.2018.00759
Russo, Ethan B. “Clinical Endocannabinoid Deficiency Reconsidered: Current Research Supports the Theory in Migraine, Fibromyalgia, Irritable Bowel, and Other Treatment-Resistant Syndromes.” Cannabis and cannabinoid research vol. 1,1 154-165. 1 Jul. 2016, doi:10.1089/can.2016.0009
Singh, Kuldeep et al. “Emerging Therapeutic Potential of Cannabidiol (CBD) in Neurological Disorders: A Comprehensive Review.” Behavioural neurology vol. 2023 8825358. 12 Oct. 2023, doi:10.1155/2023/8825358
Smiarowska, Małgorzata et al. “Cannabis and cannabinoids: pharmacology and therapeutic potential.” Neurologia i neurochirurgia polska vol. 56,1 (2022): 4-13. doi:10.5603/PJNNS.a2022.0015. This article is available in open access under Creative Common Attribution-Non-Commercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) license,







