Organophosphate, a commonly used pesticide, has profound effects on the body, which can be long-lasting as it accumulates in adipose tissue.
Organophosphate causes acetylcholine overactivity, which can lead to neurotoxicity, severe muscle paralysis, seizures, cardiorespiratory depression, and even death. Due to its generation of reactive oxygen species, organophosphate can deplete glutathione and superoxide dismutase, disarming antioxidant defense systems and increasing oxidative stress.
Organophosphate can directly damage pancreatic beta cells and contribute to elevated lipase, amylase, insulin, and blood glucose. It can impair glycogen synthesis, increase gluconeogenesis, promote insulin resistance, and cause type 2 diabetes (Chung 2021).
However, this is not new news.
Previous human and animal studies have found that exposure to organophosphate and organochlorine pesticides can increase diabetes risk. A 2008 NIH news release confirmed that long-term exposure can cause diabetes in those applying pesticides (NIH 2008). The study found that the odds of developing diabetes increased by 94%, 63%, and 51% with at least 100 lifetime days of exposure to heptachlor, chlordane, and aldrin, respectively. Exposure to dichlorvos, trichlorfon, alachlor, and cyanazine was also associated with diabetes risk (Montgomery 2008).
Pesticide contamination of groundwater is associated with diabetes risk as well. A case-control study was conducted on 390 individuals with no history of diabetes or pesticide. Results indicated that those consuming the highest amount of organochlorine pesticides (OCPs) had the highest risk of diabetes and prediabetes and were more likely to consume groundwater versus tap water or filtered water (e.g., gravity or reverse osmosis). Levels of OCPs, including DDT, were significantly higher in groundwater versus tap or filtered water and significantly higher in the blood of those with T2DM or pre-diabetes versus normal glucose tolerance. The following blood biomarkers results were evident in those diagnosed with T2DM: mean HbA1C 7.31%, fasting glucose 136 mg/dL, postprandial glucose 286 mg/dL, fasting insulin 24.9 mIU/L, total cholesterol 165 mg/dL, triglycerides 137 mg/dL, and HDL-cholesterol 42.8 mg/dL. Interestingly, total cholesterol levels were significantly lower in T2DM than in normal glucose tolerance (Tyagi 2021).
Postulated molecular mechanisms of new-onset diabetes mellitus after organophosphate pesticide exposure.
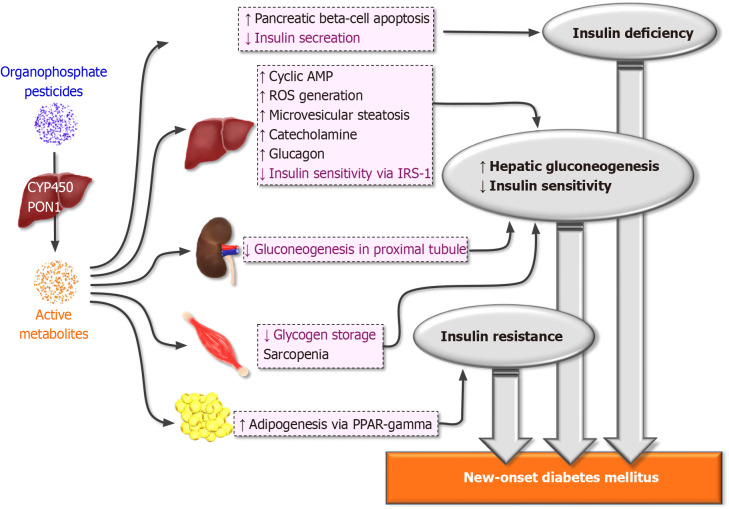
Organophosphate pesticides are metabolized in the liver to toxic derivatives via cytochrome P450 via a first-pass effect. Paroxonase isoform 1 serves as the enzyme handling hydroxylation and cleavage of the toxic form. The active metabolite might induce new-onset diabetes mellitus via pancreatic beta cell damage and disturb the homeostasis of gluconeogenesis and insulin sensitivity.
Organophosphates could directly induce apoptosis of pancreatic beta cells by activating nuclear factor-κappa beta, and therefore, insulin secretion may be hampered. Beyond pancreatic cells, gluconeogenesis within the liver could be activated by reactive oxidative species generation and inflammation induced by microvesicular steatosis, enhanced cyclic adenosine monophosphate generation, excessive catecholamine and abated insulin sensitivity of hepatocytes via insulin receptor substrate-1.
Distal organ damage by organophosphates may also disturb the homeostasis of gluconeogenesis. In organophosphate-related acute kidney injury, gluconeogenesis within the proximal tubules is disturbed. Decreased proximal gluconeogenesis exacerbates excessive hepatic gluconeogenesis. In skeletal muscle, sarcopenia mediated by intermediate syndrome might reduce glycogen storage within skeletal muscle, which may induce hyperglycemia.
Organophosphates also deposit within adipose tissue and therefore exacerbate adipogenesis by activating peroxisome proliferator-activated receptor-gamma. Excessive adipose tissue might enhance insulin resistance and further hasten the development of new-onset diabetes mellitus. CYP450: Cytochrome P450; PON1: Paroxonase isoform 1; ROS: Reactive oxidative species; AMP: Adenosine monophosphate; IRS-1: Insulin receptor substrate-1; PPAR: Peroxisome proliferator-activated receptor.
Source: Chung, Ya-Ling et al. “Organophosphate pesticides and new-onset diabetes mellitus: From molecular mechanisms to a possible therapeutic perspective.” World journal of diabetes vol. 12,11 (2021): 1818-1831. doi:10.4239/wjd.v12.i11.1818 Distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license
Beyond diabetes
The metabolic disruption and disease risk caused by pesticides extends beyond diabetes to other disorders, including cancer, kidney failure, reproductive disorders, birth defects, autoimmune dysfunction, and respiratory, neurodegenerative, and cardiovascular diseases (Czajka 2019).
Researchers suggest that combating oxidative stress may help reduce the damaging effects of pesticides. For example, the use of N-acetylcysteine (NAC) can promote glutathione synthesis and reduce malondialdehyde (MDA) production (Chung 2021).
Because contamination of air, water, and food with pesticides is widespread, it is vital to reduce exposure as much as possible and support the body’s detoxification systems to minimize adverse effects. The following foods and nutrients can help to “lighten the load” (Hyman 2010):
- Curcuminoids
- g., turmeric, curry
- Cruciferous vegetables
- g., arugula, bok choy, broccoli, Brussels sprouts, cabbage collards, kale, kohlrabi, mustard greens, radishes, rutabaga, turnips, wasabi, watercress
- Glutathione
- Green tea
- N-acetylcysteine
- Phytonutrients, phytochemicals
- Sulfur-containing foods
- g., garlic, onions, and eggs.
- Vitamins and minerals
- g., vitamin C, B6, B12, folate, zinc, and selenium
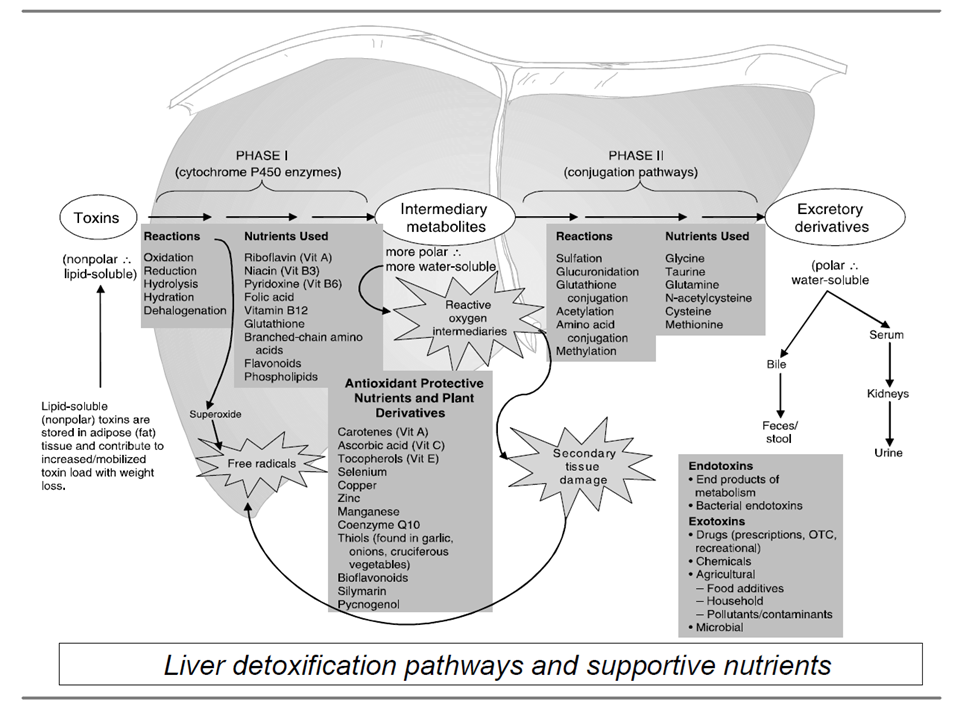
Source: Institute for Functional Medicine. Applying Functional Medicine in Clinical Practice.
ODX Optimal Takeaways
Pesticides have become ubiquitous in the environment, leading to air, water, and food contamination.
Lighten the load as much as possible by consuming organically grown produce and animal products and using adequately filtered water.
Support the body’s detoxification systems with whole plant-based foods, especially vegetables, fruits, herbs, and spices.
Supplement with micronutrients, vitamins, and minerals as needed.
References
Chung, Ya-Ling et al. “Organophosphate pesticides and new-onset diabetes mellitus: From molecular mechanisms to a possible therapeutic perspective.” World journal of diabetes vol. 12,11 (2021): 1818-1831. doi:10.4239/wjd.v12.i11.1818
Czajka, Magdalena et al. “Organophosphorus pesticides can influence the development of obesity and type 2 diabetes with concomitant metabolic changes.” Environmental research vol. 178 (2019): 108685. doi:10.1016/j.envres.2019.108685
Hyman, Mark A. “Environmental toxins, obesity, and diabetes: an emerging risk factor.” Alternative therapies in health and medicine vol. 16,2 (2010): 56-8.
NIH News Release. Long-term Pesticide Exposure May Increase Risk of Diabetes. June 4, 2008. re: Montgomery 2008
Montgomery, M P et al. “Incident diabetes and pesticide exposure among licensed pesticide applicators: Agricultural Health Study, 1993-2003.” American journal of epidemiology vol. 167,10 (2008): 1235-46.
Tyagi, Shipra et al. “High levels of organochlorine pesticides in drinking water as a risk factor for type 2 diabetes: A study in north India.” Environmental pollution (Barking, Essex : 1987) vol. 271 (2021): 116287. doi:10.1016/j.envpol.2020.116287







