Optimal Takeaways
Calcium is essential to bone metabolism, nerve transmission, coagulation, enzyme activity, myocardial function, and muscle contraction. Ionized calcium is free, unbound, and bioavailable. It makes up about 40% of total blood calcium, with the remainder bound primarily to albumin.
A low ionized calcium may be associated with tetany, seizures, paresthesias, alkalosis, hypoparathyroidism, and increased non-cardiovascular mortality risk. An elevated ionized calcium may be associated with primary hyperparathyroidism, malignancy, renal failure, acidosis, bone breakdown, cardiovascular disease, and mortality.
Standard Range: 4.7 – 5.5 mg/dL (1.18 – 1.38 mmol/L)
The ODX Range: 4.7 – 5 .1 mg/dL (1.18 – 1.27 mmol/L)
Low ionized calcium is associated with neuromuscular excitability, tetany, seizures, paresthesias, hypoparathyroidism, parathyroid gland resection, acute pancreatitis, Chvostek and Trousseau signs (Baird 2011), alkaline pH, foscarnet drug therapy, blood transfusion, respiratory alkalosis (Goyal 2023), worsening of intracerebral hematoma (Hamroun 2020), increased all-cause and specific-cause mortality risk including cancer but not cardiovascular mortality (Kobylecki 2022).
High ionized calcium is associated with primary hyperparathyroidism, malignancy, excess 1,25-dihydroxyvitamin D, granulomatous disorders, renal failure, osteoporosis due to bone breakdown (Baird 2011), severe acidosis (Goyal 2023), ischemic cardiovascular changes (Reid 2016), and cardiovascular mortality (Kobylecki 2022).
Overview
Calcium is the most abundant mineral in the body, primarily in the bone. However, a small amount is found extracellularly and intracellularly, where it plays a role in vital processes, including nerve transmission, enzyme activity, myocardial function, coagulation (Sadiq 2023), and muscle contraction. Only 1% of total body calcium is found in circulation, where 50% is bound to protein (primarily albumin), 10% is ionic-bound (in complexes of phosphate, carbonate, and oxalate), and 40% is “free” active bioavailable ionized calcium (Hamroun 2020).
Blood levels of ionized calcium are tightly controlled through a complex hormonal process involving the gastrointestinal tract, kidney, and bone. Low ionized calcium triggers the release of parathyroid hormone (PTH), which increases renal absorption of calcium, stimulates bone to release calcium into circulation, and increases renal conversion of vitamin D to its active 1,25(OH)2D calcitriol form. Calcitriol then signals the intestines to increase calcium absorption. A high calcium intake will suppress PTH, reducing calcitriol synthesis and gastrointestinal calcium absorption, while insufficient calcium intake may lead to bone resorption. Kidney failure decreases calcium excretion but also reduces calcitriol production and calcium absorption. Overall, this dynamic process maintains a precise level of ionized calcium in circulation, potentially at the expense of bone. Therefore, serum ionized calcium does not fully reflect or assess total body calcium balance (Hill 2017).
Total serum calcium reflects bound and free ionized calcium in circulation and may be sufficient for screening and general assessment. Total serum calcium often correlates with ionized calcium in healthy individuals and should be adequate for clinical evaluation. However, changes in serum albumin, pH, medication, or albumin-bound fatty acids can alter this correlation, leading to misclassification of calcium status using total calcium or *adjusted calcium (calculated if albumin is low). Ionized calcium measurement may be more appropriate under these circumstances and is the gold standard for known calcium metabolism alterations or during critical illness. Ionized hypercalcemia is uncommon but can be associated with hyperparathyroidism, malignancies, kidney stones, renal failure, osteoporosis, and excess 1,25-dihydroxy vitamin D. Ionized hypocalcemia may be more common and present with neuromuscular excitability (Chvostek and Trousseau signs), seizure, tetany, and paresthesias. Calcium measurement should be repeated and confirmed before therapeutic intervention, especially in critical illness (Baird 2011).
Ionized calcium may decrease transiently following moderate-intensity physical activity because of increased lactate and acidity associated with exercise; following meals because of increased binding of calcium with proteins and other anions; and due to circadian rhythm changes in which an ionized calcium nadir occurs in late afternoon. Acid-base changes should also be accounted for. These include a decrease in ionized calcium when pH increases, e.g., with hyperventilation-induced respiratory pH. Ionized calcium can increase with acidity and decreased pH. An estimated 5% change in ionized calcium is observed for each 0.1 variation in pH unit. Limited research suggests that altered ionized calcium levels may be associated with male infertility, preeclampsia, and depression, though these associations require further study. Currently, measuring ionized calcium is not indicated for most of the population. However, it would be prudent to measure ionized calcium in those suspected of hyperparathyroidism, those with chronic kidney disease, cancer, chemotherapy treatment, and those in intensive care (Hamroun 2020).
Low ionized calcium has been associated with increased mortality risk in the general population, while increased ionized calcium is associated with cardiovascular mortality risk, though causation has not been established. Evaluation of 106,768 individuals from the Copenhagen General Population Study found each 0.40 mg/dL (0.1 mmol/L) below 4.84 mg/dL (1.21 mmol/L), risk of all-cause mortality increased by 23%, cancer mortality increased by 29%, and other non-cardiovascular mortality increased by 24%. Cardiovascular mortality risk rose by 17% with each 0.40 mg/dL (0.1 mmol/L) above 4.84 mg/dL (1.21 mmol/L), possibly in relation to increased mineralization of vascular smooth muscle cells and promotion of atherosclerosis (Kobylecki 2022).
A higher serum calcium within the standard range has been associated with increased cardiovascular risk, possibly related to calcium’s potential role in promoting coagulation and calcification of soft tissue. Research findings indicate that calcified plaque was associated with higher serum calcium, while uncalcified plaque was not. Some research has associated higher ionized calcium with ischemic heart disease in healthy subjects and ischemic brain changes in depressed individuals (Reid 2016).
Ionized calcium is more sensitive than total or adjusted total calcium for diagnosing primary hyperparathyroidism, characterized by hypercalcemia and elevated or unsuppressed serum PTH. An observational, retrospective, cross-sectional study of 5,490 subjects with suspected bone or calcium disorders revealed discordance between total and ionized calcium in 12.5% of this population. Dependence on total serum calcium alone would have missed 45% of cases of hypercalcemia identified by measuring ionized calcium. Isolated ionized hypercalcemia was found in 130 of 315 cases of PTH-dependent hypercalcemia and 34 of 143 cases of histologically proven parathyroid disease. Researchers note that measurement of ionized calcium is more labor-intensive and expensive than total calcium. Further mathematical adjustment of ionized calcium to pH 7.4 may need to be performed to account for minor pH issues associated with sample handling (Ong 2012).
Evaluation of ionized calcium in 33,255 hospitalized patients revealed a U-shaped curve between serum levels, in-patient, and 1-year mortality rates. Researchers note that in-hospital mortality increased with ionized calcium of 4.59 mg/dL (1.15 mmol/L) or below, and 1-year mortality increased at 4.39 mg/dL (1.10 mmol/L) or below. The in-patient and 1-year mortality increased with ionized calcium of 5.20 mg/dL (1.3 mmol/L) or above (Thongprayoon 2020).
Certain medications can alter calcium levels but may affect total and ionized calcium differently and should be evaluated individually.
*Adjusted total calcium equations
Total calcium can be corrected or “adjusted” for low albumin to reflect actual calcium status in most patients better using the formulae:
- Adjusted/corrected total calcium (mg/dL) = Measured Total calcium (in mg/dL) + 0.8 X [4 − albumin mg/dL) ] (Baird 2011)
- Adjusted/corrected total calcium (mmol/L) = Measured Total calcium (in mmol/L) + 0.02 [40 - albumin (in g/L)] (Ong 2020).
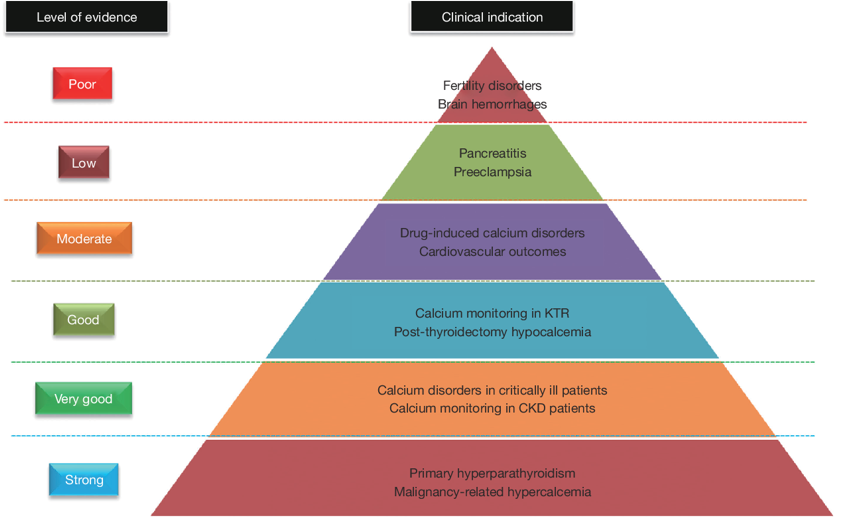
Clinical usefulness of ionized calcium measurement, based on level of evidence
Complexity of ionized calcium measurement and interpretation
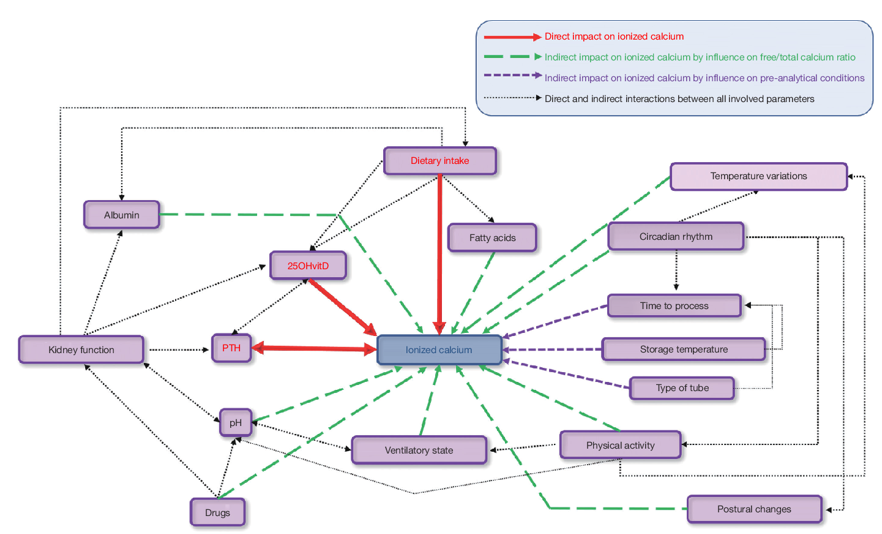
Source: Hamroun, Aghilès, et al. "Ionized calcium: analytical challenges and clinical relevance." J Lab Precis Med 5 (2020): 22. his is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), https://creativecommons.org/licenses/by-nc-nd/ https://www.researchgate.net/profile/Guillaume-Grzych/publication/342550301_Ionized_calcium_analytical_challenges_and_clinical_relevance/links/5efafac4a6fdcc4ca43d9ffb/Ionized-calcium-analytical-challenges-and-clinical-relevance.pdf
References
Baird, Geoffrey S. “Ionized calcium.” Clinica chimica acta; international journal of clinical chemistry vol. 412,9-10 (2011): 696-701. doi:10.1016/j.cca.2011.01.004
Goyal, Abhinav, et al. “Hypocalcemia.” StatPearls, StatPearls Publishing, 15 October 2023.
Hamroun, Aghilès, et al. "Ionized calcium: analytical challenges and clinical relevance." J Lab Precis Med 5 (2020): 22.
Hill Gallant, Kathleen M, and David M Spiegel. “Calcium Balance in Chronic Kidney Disease.” Current osteoporosis reports vol. 15,3 (2017): 214-221. doi:10.1007/s11914-017-0368-x
Kobylecki, Camilla J et al. “Low Plasma Ionized Calcium Is Associated With Increased Mortality: A Population-based Study of 106 768 Individuals.” The Journal of clinical endocrinology and metabolism vol. 107,7 (2022): e3039-e3047. doi:10.1210/clinem/dgac146
Ong, Gregory S Y et al. “The importance of measuring ionized calcium in characterizing calcium status and diagnosing primary hyperparathyroidism.” The Journal of clinical endocrinology and metabolism vol. 97,9 (2012): 3138-45. doi:10.1210/jc.2012-1429
Pagana, Kathleen Deska, et al. Mosby's Diagnostic and Laboratory Test Reference. 16th ed., Mosby, 2022.
Sadiq, Nazia M., et al. “Hypercalcemia.” StatPearls, StatPearls Publishing, 4 September 2023.
Reid, I R et al. “Circulating calcium concentrations, vascular disease and mortality: a systematic review.” Journal of internal medicine vol. 279,6 (2016): 524-40. doi:10.1111/joim.12464
Thongprayoon, Charat et al. “Hospital mortality and long-term mortality among hospitalized patients with various admission serum ionized calcium levels.” Postgraduate medicine vol. 132,4 (2020): 385-390. doi:10.1080/00325481.2020.1728980







