Melatonin is a hormone that is produced mainly in the pineal gland but is also synthesized by the enterochromaffin cells in the GI tract.
Although it is most commonly associated with sleep, it is found throughout the body, where it helps fight oxidative stress, supports immune function, modulates inflammatory cytokines, and regulates mitochondrial homeostasis. Here are some intriguing facts about this multipurpose molecule from an excellent article in the journal Nutrients authored by Dr. Deanna Minich entitled “Is Melatonin the "Next Vitamin D"?: A Review of Emerging Science, Clinical Uses, Safety, and Dietary Supplements.” (Minich 2022):
- Melatonin is found in just about all bodily fluids, including saliva, urine, synovial fluid, and bile.
- Melatonin has been found in many tissues other than the pineal gland and gut mucosa, including the brain, retina, lens, cochlea, trachea, skin, liver, kidney, thyroid, pancreas, thymus, spleen, and reproductive tissues.
- Production of melatonin can be influenced by
- Illness
- Diet
- Environmental factors such as bright light at night
- Medication use
- Lifestyle
- In its antioxidant capacity, melatonin is able to quench as many as 10 reactive oxygen and nitrogen species compared to many other antioxidant compounds that only quelch a few.
- Broad therapeutic benefits in the GI tract include melatonin’s role in oral care and digestive function, periodontal inflammation, post-dental surgery, and antioxidant protection against dental materials.
- On average, the pineal gland produces between 0.1 and 0.9 mg of melatonin per day.
- Production gradually declines as people age, starting in the late twenties to the fifties, with production leveling at approximately 30 pg/mL.
- Melatonin imbalance may be associated with
- Stressful events
- Oxidative stress
- A highly processed, inflammatory diet
- Jet lag
- Shift work
- Overuse of artificial light at night (e.g., from cell phones, computers, and fluorescent/LED light)
- Challenges to circadian rhythm due to environmental or seasonal changes
- Melatonin is derived from serotonin using 5-hydroxytryptophan (5-HTP) and tryptophan
- The melatonin-serotonin pathway accounts for approximately 5% of dietary tryptophan degradation, while the kynurenic pathway accounts for approximately 95% of dietary tryptophan degradation.
- Kynurenine is a byproduct or metabolite produced when tryptophan is converted to niacin.
- The kynurenic pathway is an essential process needed to convert tryptophan into nicotinamide adenine dinucleotide (NAD+) for cellular energy.
- Under states of stress and high cortisol, tryptophan’s conversion to serotonin and melatonin is shunted to kynurenine.
- High concentration levels of kynurenine in the brain are present in instances of depression.
- Broad therapeutic benefits in the GI tract include melatonin’s role in oral care and digestive function, periodontal inflammation, post-dental surgery, and antioxidant protection against dental materials.
- Enterochromaffin cells are not regulated by light and dark but appear affected by food intake and digestion
- Levels of gut melatonin can be anywhere from 10 to 100 times greater than melatonin in blood serum levels.
- Melatonin may work synergistically with Vitamin D as they both
- Act as hormones
- Affect multiple systems through their immune-modulating, anti-inflammatory functions
- Are found in the skin
- Are responsive to sunlight (vitamin D) and darkness (melatonin)
-
Melatonin is found in a number of plant-based foods and some animal-based foods and can contribute to circulating melatonin and antioxidant capacity. However, the amount found in food is not considered adequate to meet repletion needs.
-
Melatonin supplementation is considered safe in general. However, dosage and sources should be individualized, and potential contraindications must be taken into account, including the use of medications metabolized via cytochrome enzymes.
-
Supplement sources include synthetic, animal, and plant (phytomelatonin)
-
- Melatonin can bind the vitamin D receptor (VDR), resulting in an enhancement of vitamin D’s signaling effects and subsequent cellular activities
- Melatonin may work synergistically with Vitamin D as they both
- Act as hormones
- Affect multiple systems through their immune-modulating, anti-inflammatory functions
- Are found in the skin
- Are responsive to sunlight (vitamin D) and darkness (melatonin)
-
More clinical research is warranted to better understand melatonin’s effects from dietary intake and how it is influenced by gene variants and receptors, as well as its metabolism, metabolites, and laboratory assessment.
-
From a clinical perspective, assessing one’s levels of systemic melatonin is difficult.
-
Salivary melatonin samples are collected in the evening to determine the time of melatonin onset, called “dim light melatonin onset” (DLMO).
-
Urinary melatonin metabolite 6-sulfatoxymelatonin can be measured in morning urine to assess accumulated melatonin over the night.
-
Blood samples can also be collected, showing melatonin levels in real-time, and is a more sensitive measure, so preferred in cases of low melatonin.
-
Vitamin D and melatonin as light and dark sensors with shared functions.
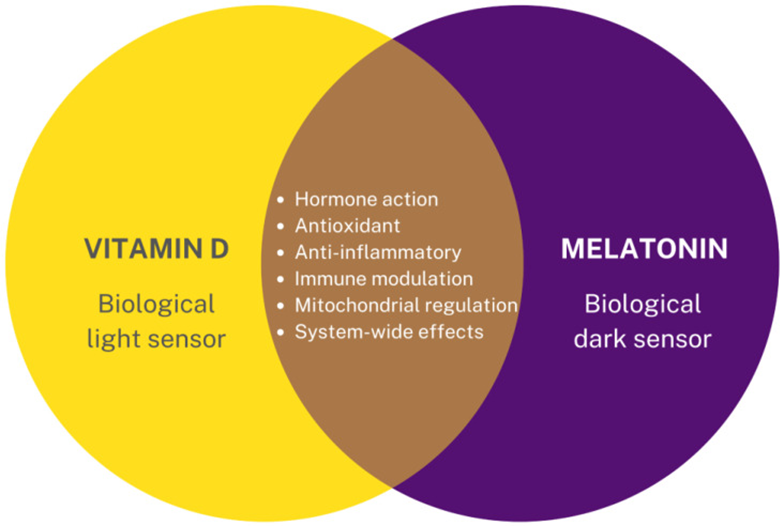
Source: Minich, Deanna M et al. “Is Melatonin the "Next Vitamin D"?: A Review of Emerging Science, Clinical Uses, Safety, and Dietary Supplements.” Nutrients vol. 14,19 3934. 22 Sep. 2022, doi:10.3390/nu14193934 This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/). Graphic created using https://Canva.com accessed 27 July 2022.
Monitoring Melatonin Status
The use of blood levels to monitor melatonin status may be complex due to the significant number of factors affecting its production and utilization. Although 80% of melatonin is produced at night, the amount of nocturnal secretion may be determined genetically and vary greatly between individuals. However, an individual's circadian profile for melatonin may be reproducible over a six-week period of monitoring in the same person. In general, daytime serum concentrations of melatonin remain low at approximately (10-20 pg/ml), while nighttime concentrations increase significantly to 80-120 pg/mL with a peak concentration between midnight and 3 am (Karasek 2006).
References ranges established by Quest Diagnostics are as follows:
References
Karasek, M, and K Winczyk. “Melatonin in humans.” Journal of physiology and pharmacology : an official journal of the Polish Physiological Society vol. 57 Suppl 5 (2006): 19-39.
Minich, Deanna M et al. “Is Melatonin the "Next Vitamin D"?: A Review of Emerging Science, Clinical Uses, Safety, and Dietary Supplements.” Nutrients vol. 14,19 3934. 22 Sep. 2022, doi:10.3390/nu14193934 This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Quest Diagnostics. Melatonin. https://testdirectory.questdiagnostics.com/test/test-detail/91899/melatonin-serumplasma?cc=MASTER







