Standard reference ranges may vary slightly for older versus younger adults, depending on the biomarker and, in some cases, the lab. Pediatric ranges are completely separate for many biomarkers and should be assessed separately as they reflect growth and development as well as potential pathological changes.
An in-depth Canadian Health Measures Survey (CHMS) of reference ranges for 24 biomarkers from 12,000 apparently healthy individuals 3-79 of age was conducted. Adulthood was defined as 18-49 years and geriatric was defined as 50-79 years. In general, the analysis found (Adeli 2015 Biochemical marker):
However, the issue is more complex than just measuring chronological age, as one’s “phenotypic” or biological age may be different than one’s fixed chronological age. Susceptibility to age-related disease and mortality can vary significantly between individuals of the same chronological age depending on diet, lifestyle, and epigenetics. Biological age can be evaluated using blood biomarkers, including albumin, creatinine, glucose, CRP, WBC count, lymphocyte percentage, MCV, RDW, and alkaline phosphatase. Acceleration in biological age ultimately correlates with increases in CRP, insulin, glucose, triglyceride, and waist-to-hip ratio (Levine 2018).
Measuring biological age may more accurately assess an individual's actual risk of adverse outcomes. Research suggests that measuring frailty can help evaluate biological age and identify accelerated aging. Frailty results from multilevel deterioration of physiological systems in the body. Phenotypic frailty includes at least one of the following three criteria: weight loss, low physical activity, exhaustion, weak grip, and/or slow gait.
A second model of frailty, the deficit accumulation model, implies that the accumulation of health deficits at any age increases the range and occurrence of adverse outcomes. Health deficits can be associated with laboratory biomarkers, signs and symptoms, functional impairments, and disease states. The degree of frailty can help predict morbidity and mortality from a specific disease state or condition. The Clinical Frailty Scale (CFS) reflects the cumulative impact of health deficits associated with cognitive impairment, comorbidities, disability, mobility, and physical activity. The CFS has been validated in individuals over the age of 65. The CFS can be improved with nutrition and exercise programs, as well as positive interventions in the medical, psychological, functional, and social needs of an individual. Nutrition and lifestyle facilitate epigenetic changes to DNA, i.e., changes that modify DNA but don’t change its sequencing. DNA methylation is an example of an epigenetic change that is influenced by both environmental and genetic factors. Epigenetic “age” is directly related to social and lifestyle behaviors, including high fish intake, moderation in alcohol consumption, and higher education (Diebel 2021).
The European MARK-AGE population study of 3,200 subjects suggests a comprehensive set of biomarkers that may help evaluate biological age, including (Burkle 2015):
Interrelationships within and among biological processes
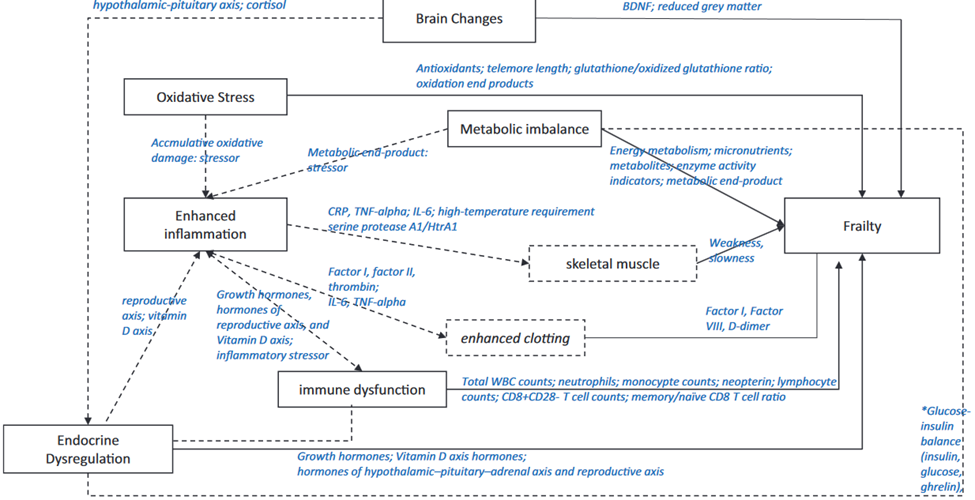
BDNF = brain-derived neurotrophic factor; CRP = C-reactive protein; TNF-a = tumor necrosis factor-a; IL-6 = interleukin-6; WBC = white blood cell
Source: Wang, Jinjiao et al. “Biological Processes and Biomarkers Related to Frailty in Older Adults: A State-of-the-Science Literature Review.” Biological research for nursing vol. 21,1 (2019): 80-106. doi:10.1177/1099800418798047
Malnutrition can be a factor in biological aging and is associated with significantly decreased albumin, prealbumin, total protein, hemoglobin, total cholesterol, and BMI (Zhang 2017). Additional factors can contribute to biological aging and health status and should be considered in a comprehensive assessment, including biomarkers of endocrine function, immune function, cognitive function, and physical capability (Lara 2015).
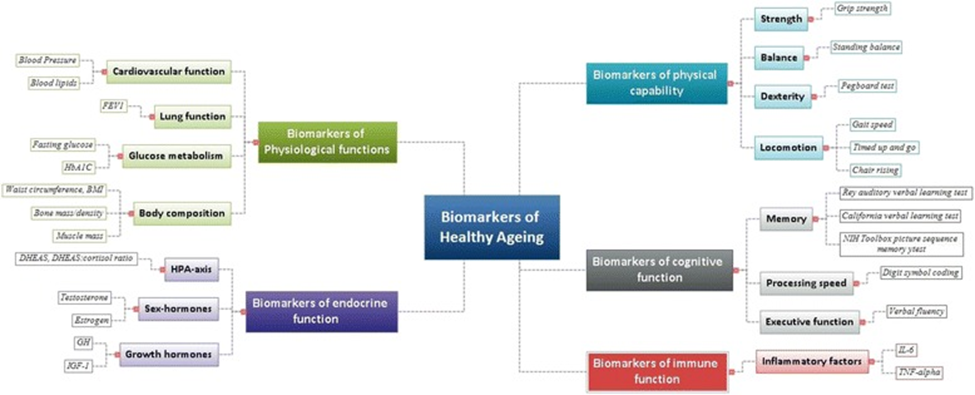
Source: Lara, Jose et al. “A proposed panel of biomarkers of healthy ageing.” BMC medicine vol. 13 222. 15 Sep. 2015, doi:10.1186/s12916-015-0470-9 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/),
Although there are no currently defined optimal biomarker ranges for the age group designated as “geriatric,” there are a number of biomarkers that can help evaluate someone’s “biological” age and disease risk, regardless of their fixed chronological age.
Evaluating these biomarkers within a functional matrix range can help identify accelerated aging, advanced biological age, and trends toward dysfunction:
Adeli, Khosrow et al. “Biochemical marker reference values across pediatric, adult, and geriatric ages: establishment of robust pediatric and adult reference intervals on the basis of the Canadian Health Measures Survey.” Clinical chemistry vol. 61,8 (2015): 1049-62. doi:10.1373/clinchem.2015.240515
Adeli, Khosrow et al. “Complex reference values for endocrine and special chemistry biomarkers across pediatric, adult, and geriatric ages: establishment of robust pediatric and adult reference intervals on the basis of the Canadian Health Measures Survey.” Clinical chemistry vol. 61,8 (2015): 1063-74. doi:10.1373/clinchem.2015.240523
Burkle, Alexander et al. “MARK-AGE biomarkers of ageing.” Mechanisms of ageing and development vol. 151 (2015): 2-12. doi:10.1016/j.mad.2015.03.006
Diebel, Lucas W M, and Kenneth Rockwood. “Determination of Biological Age: Geriatric Assessment vs Biological Biomarkers.” Current oncology reports vol. 23,9 104. 16 Jul. 2021, doi:10.1007/s11912-021-01097-9
Lara, Jose et al. “A proposed panel of biomarkers of healthy ageing.” BMC medicine vol. 13 222. 15 Sep. 2015, doi:10.1186/s12916-015-0470-9
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (
Levine, Morgan E et al. “An epigenetic biomarker of aging for lifespan and healthspan.” Aging vol. 10,4 (2018): 573-591. doi:10.18632/aging.101414
Wang, Jinjiao et al. “Biological Processes and Biomarkers Related to Frailty in Older Adults: A State-of-the-Science Literature Review.” Biological research for nursing vol. 21,1 (2019): 80-106. doi:10.1177/1099800418798047
Zhang, Zhiying et al. “Evaluation of Blood Biomarkers Associated with Risk of Malnutrition in Older Adults: A Systematic Review and Meta-Analysis.” Nutrients vol. 9,8 829. 3 Aug. 2017, doi:10.3390/nu9080829