Nutrition screening should be performed by a specialist (e.g., a dietitian) using subjective and objective parameters such as clinical history, physical examination, body composition measurements, functional assessment, and laboratory values.
A set of laboratory parameters in the clinical routine (e.g., complete blood count, lipid profile, electrolytes, liver parameters) may provide valuable information about a patient’s nutritional status (e.g., proof of nutrient deficiency, information about the etiology of malnutrition, follow-up nutritional therapy), about the severity and activity of the disease, and about changes in body composition.
Laboratory values—particularly in chronically malnourished patients—may help to detect deficiencies in vitamins (C, D, E, K, thiamin, B6, B12, and folate) and trace elements (zinc, selenium, and iron) and help to monitor current substitution therapies. In the early phase of refeeding, potassium, phosphate, and magnesium deficiencies may occur, potentially leading to severe complications (e.g., refeeding syndrome); hence, there is a need for close monitoring of these electrolytes.
|
lAB vALUE |
Nutrition Independent Factors |
1/2 -Life |
Appropriate to Detect |
Appropriate to Monitor Nutritional Therapy |
|---|---|---|---|---|
|
Albumin |
↑ dehydration |
20 d |
+/++ |
Not appropriate due to high suggestibility and long half-life |
|
↓ inflammation, infections, trauma, heart failure, edema, liver dysfunction, nephrotic syndrome |
||||
|
Not appropriate in case of anorexia and acute illness |
||||
|
Transferrin |
↑ renal failure, iron status, acute hepatitis, hypoxia |
10 d |
+ |
+ |
|
↓ inflammation, chronic infections hemochromatosis, nephrotic syndrome, liver dysfunction |
Low sensitivity and specificity |
Concentration is independent of the energy and protein intake |
||
|
Prealbumin/Transthyretin (TTR) |
↑ renal dysfunction, dehydration, corticosteroid therapy |
2 d |
++ |
++/+++ |
|
Not appropriate to detect anorexia Subnormal values within one week in case of fasting |
||||
|
One of the most appropriate proteins |
||||
|
↓ inflammation, hyperthyreosis, liver disease, overhydration |
||||
|
Retinol binding protein (RBP) |
↑ kidney failure, alcohol abuse |
12 h |
Idem prealbumin |
Idem prealbumin |
|
↓ hyperthyreosis, chronic liver diseases, vitamin A deficiency, selenium deficiency |
||||
|
Insulin-like growth factor 1 (IGF-1) |
↑ kidney failure |
24 h |
++ |
+++ |
|
More specific than retinol-binding protein and prealbumin/ transthyretin |
||||
|
↓ liver diseases, severe catabolic status, age |
Rapid decrease in fasting periods |
|||
|
Urinary creatinine |
↑ collection time >24h, infection, trauma |
- |
1 mmol of creatinine is derived from 1.9 kg of skeletal muscle mass |
Not appropriate, very slow |
|
↓ insufficient collection time, acute kidney failure |
||||
|
Lymphocytes |
↑ healing phase after infection, hematologic diseases |
- |
+ |
Not appropriate, very slow |
|
↓ sepsis, hematologic disease, immune suppressants, steroids |
Very unspecific |
Physical examination is an objective method of detecting clinical signs and symptoms of nutritional deficiencies of vitamins and minerals (e.g., poor muscle control, night vision impairment, vertical lip cracks, depression), and allows the assessment of tolerance to nutritional support (e.g., abdominal distention, vomiting, diarrhea).
Some clinical signs are specific to a specific disease or nutrient deficiency. Others are non-specific and need further tests to elucidate their etiology (Table 6). Physical examination includes the control of vital parameters, the inspection and palpation for water retention (edema and ascites), and a rough assessment of muscle mass and subcutaneous fat stores.
|
Body Region |
Signs |
Possible Deficiencies |
|---|---|---|
|
Skin |
Petechiae |
Vitamins A, C |
|
Purpura |
Vitamins C, K |
|
|
Pigmentation |
Niacin |
|
|
Edema |
Protein, vitamin B1 |
|
|
Pallor |
Folate, iron, biotin, vitamins B12, B6 |
|
|
Decubitus |
Protein, energy |
|
|
Seborrheic dermatitis |
Vitamin B6, biotin, zinc, essential fatty acids |
|
|
Unhealed wounds |
Vitamin C, protein, zinc |
|
|
Nails |
Pallor or white coloring Clubbing, spoon-shape, or transverse ridging/banding; excessive dryness, darkness in nails, curved nail ends |
Iron, protein, vitamin B12 |
|
Head/Hair |
Dull/lackluster; banding/sparse; alopecia; depigmentation of hair; scaly/flaky scalp |
Protein and energy, biotin, copper, essential fatty acid |
|
Eyes |
Pallor conjunctiva |
Vitamin B12, folate, iron |
|
Night vision impairment |
Vitamin A |
|
|
Photophobia |
Zinc |
|
|
Oral cavity |
Glossitis |
Vitamins B2, B6, B12, niacin, iron, folate |
|
Gingivitis |
Vitamin C |
|
|
Fissures, stomatitis |
Vitamin B2, iron, protein |
|
|
Cheilosis |
Niacin, vitamins B2, B6, protein |
|
|
Pale tongue |
Iron, vitamin B12 |
|
|
Atrophied papillae |
Vitamin B2, niacin, iron |
|
|
Nervous system |
Mental confusion |
Vitamins B1, B2, B12, water |
|
Depression, lethargy |
Biotin, folate vitamin C |
|
|
Weakness, leg paralysis |
Vitamins B1, B6, B12, pantothenic acid |
|
|
Peripheral neuropathy |
Vitamins B2, B6, B12 |
|
|
Ataxia |
Vitamin B12 |
|
|
Hyporeflexia |
Vitamin B1 |
|
|
Muscle cramps |
Vitamin B6, calcium, magnesium |
|
|
Fatigue |
Energy, biotin, magnesium, iron |
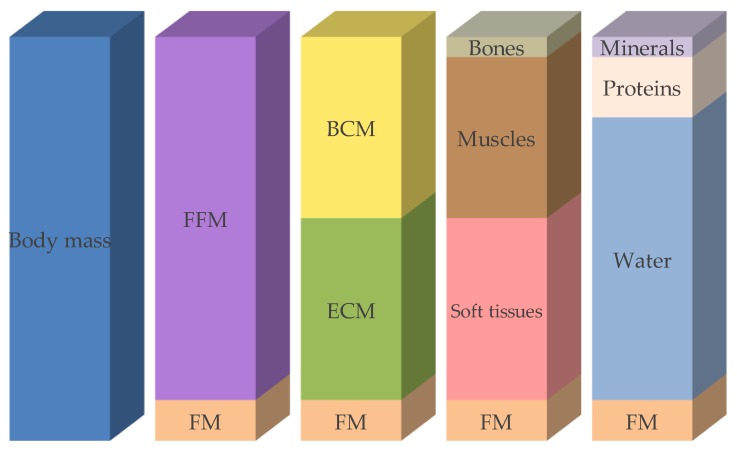
FFM: fat-free mass, FM: fat mass, BCM: body cell mass, ECM: extracellular cell mass.
|
Macronutrient |
Energy Content |
Recommended Amount/kg Body Weight/dAY |
|---|---|---|
|
Proteins |
4 kcal |
1.0–1.5 g |
|
Carbohydrates |
4 kcal |
max. 3–5 g |
|
Fats |
9 kcal |
0.8–1.5 g |
Reber, Emilie et al. “Nutritional Risk Screening and Assessment.” Journal of clinical medicine vol. 8,7 1065. 20 Jul. 2019, doi:10.3390/jcm8071065 https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/31330781/ This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Fruits, including berries, grapes, citrus, olives, etc.
Vegetables, including leafy greens, cruciferous vegetables,
orange/yellow vegetables, onions, garlic, etc.
Herbs and spices, including basil, oregano, rosemary, parsley, turmeric, cumin, ginger, etc.
Nuts, including almonds, walnuts, pistachios, etc.
Seeds, including cacao, chia, flax, pumpkin, hemp, etc.
Whole grains as tolerated, including oatmeal, non-GMO corn, etc.
Legumes as tolerated, including peanuts, non-GMO soybeans, lentils, black beans, etc.
Clean lean protein, including organic poultry and eggs, grass-fed beef and dairy, seafood, etc.
Omega-3 sources, including salmon, sardines, and occasionally tuna.
Fermented foods, including yogurt, cheese, kefir, sauerkraut, etc.
Hydrate with plenty of pure alkalized water and healthy beverages, including organic coffee, tea, homemade alkaline lemon-limeade, etc.
