There is so much more to cholesterol than meets the eye!
Apolipoproteins are structural, functional components of lipoproteins that facilitate cholesterol transport in the blood.
Research indicates that evaluating the ratio of ApoB to ApoA1 is a better tool for assessing coronary artery disease than evaluating traditional biomarkers such as total cholesterol, LDL, HDL, triglycerides, or lipid ratios, including total cholesterol/HDL-c, LDL-c/HDL-c, and TG/HDL-c.
A 5-year follow-up of 1,639 coronary heart disease patients found that those with a higher ApoB:ApoA1 ratio had
The ratio of ApoB to ApoA1 is useful in the assessment of metabolic syndrome risk as well. A 2009 health nutrition survey of 8,120 subjects in China revealed that both males and females in the highest quartile of ApoB:ApoA1 (0.98 or greater) were at a significant 4.24-fold greater risk of metabolic syndrome compared to the lowest quartile (0.61).[iii]
One study looked at metabolic syndrome risk in 100 patients with type 2 diabetes and revealed an association between ApoB:ApoA1 ratio and metabolic syndrome in men and women. In women, an association was also observed between elevated ApoB:ApoA1 and ischemic cardiomyopathy.[iv]
| Clinical Implications High | Clinical Implications Low |
| Atherosclerotic plaque [v] Cardiovascular disease risk increase [vi] Metabolic syndrome Rheumatoid arthritis [vii] Statin therapy monitoring [viii] Stroke [ix]
|
A low/desirable ApoB/Apo A-1 ratio represents decreased atherogenic ApoB and a relative increase in protective Apo A-1 |
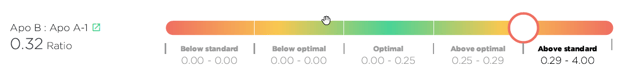
Good news! The ApoB:Apo A-1 ratio is now being automatically calculated by the Optimal DX software if both the ApoB and Apo A-1 are added into the system. No need to do any conversions as the software will do this for you and will now show the result in the Blood Test Results Report:
However, if you simply want to do the calculation manually then please follow these instructions:
The ApoB:Apo A-1 ratio is calculated by dividing the ApoB result by the Apo A-1result.
Here's an example:
ApoB is 105 and the Apo A-1 is 95: 105/ 95= 1.11
So, the ApoB:Apo A1 Ratio in this example is 1.11
[i] Lima, Luciana Moreira et al. “Apo B/apo A-I ratio and cardiovascular risk prediction.” Arquivos brasileiros de cardiologia vol. 88,6 (2007): e187-90. [R]
[ii] Tian, Min et al. “Comparison of Apolipoprotein B/A1 ratio, Framingham risk score and TC/HDL-c for predicting clinical outcomes in patients undergoing percutaneous coronary intervention.” Lipids in health and disease vol. 18,1 202. 19 Nov. 2019, [R]
[iii] Jing F, Mao Y, Guo J, et al. The value of Apolipoprotein B/Apolipoprotein A1 ratio for metabolic syndrome diagnosis in a Chinese population: a cross-sectional study. Lipids Health Dis. 2014;13:81. Published 2014 May 14. [R]
[iv] Reynoso-Villalpando, Gabriela Lizet et al. “ApoB/ApoA1 ratio and non-HDL-cholesterol/HDL-cholesterol ratio are associated to metabolic syndrome in patients with type 2 diabetes mellitus subjects and to ischemic cardiomyopathy in diabetic women.” Endocrinologia, diabetes y nutricion vol. 66,8 (2019): 502-511. [R]
[v] Panayiotou, A et al. “ApoB/ApoA1 ratio and subclinical atherosclerosis.” International angiology : a journal of the International Union of Angiology vol. 27,1 (2008): 74-80. [R]
[vi] Walldius, Göran et al. “The apoB/apoA-I ratio is better than the cholesterol ratios to estimate the balance between plasma proatherogenic and antiatherogenic lipoproteins and to predict coronary risk.” Clinical chemistry and laboratory medicine vol. 42,12 (2004): 1355-63. [R]
[vii] Öhman, M et al. “The apoB/apoA1 ratio predicts future cardiovascular events in patients with rheumatoid arthritis.” Scandinavian journal of rheumatology vol. 43,4 (2014): 259-64. [R]
[viii] Walldius, Göran et al. “The apoB/apoA-I ratio is better than the cholesterol ratios to estimate the balance between plasma proatherogenic and antiatherogenic lipoproteins and to predict coronary risk.” Clinical chemistry and laboratory medicine vol. 42,12 (2004): 1355-63. [R]
[ix] Tamang, Hem Kumar et al. “Apo B/Apo A-I Ratio is Statistically A Better Predictor of Cardiovascular Disease (CVD) than Conventional Lipid Profile: A Study from Kathmandu Valley, Nepal.” Journal of clinical and diagnostic research : JCDR vol. 8,2 (2014): 34-6. [R]